Transducer Selection
Transducer characteristics, such as frequency and shape, determine ultrasound image quality. The transducer frequencies used
for peripheral nerve blocks range from 3-15 MHz. Linear and curvilinear (or curved) transducers are most useful for nerve
imaging to provide high resolution images. Sector phased array transducers may also be used but the images are more "grainy".
Modern transducers are broad bandwidth transducers that are designed to generate more than one frequency. For example, a L 5-12
MHz transducer can generate waves ranging in frequency from 5-12 MHz. With broad bandwidth transducers, the operator can select the
examination frequency to match the target requirement. The resonance frequency is the one frequency at which the piezoelectric transducer
is most efficient in converting electrical energy to acoustic energy and vice versa. The resonance frequency is determined by the
thickness of the piezoelectric element.

For superficial structures (e.g. nerves in the interscalene, supraclavicular and axillary regions), it is ideal to use high frequency transducers greater than or equal to 7 MHz. Transducers in the range of 10-15 MHz are preferred but depth of penetration is often limited to 2-3 cm below the skin surface.
For visualization of deeper structures (e.g. in the infraclavicular and popliteal regions), it may be necessary to use a lower frequency transducer (less than or equal to 7 MHz) because it offers ultrasound penetration of 4-5 cm or more below the skin surface. However, the image resolution is often inferior to that obtained with a higher frequency transducer.
Linear transducers less than or equal to 5 cm wide are available for high frequency transducers. Smaller transducers, i.e., transducers with smaller footprints are useful for detailed scanning where the patient's anatomy prohibits the use of bulkier transducers (e.g., the supraclavicular region where there is limited access). Curved transducers are best suited for scanning whenever a wide field of view is required.
It is important to remember that:
high frequency = high spatial resolution but limited depth of penetration
low frequency = greater depth of penetration but lower spatial resolution
Examples of SonoSites Transducers:
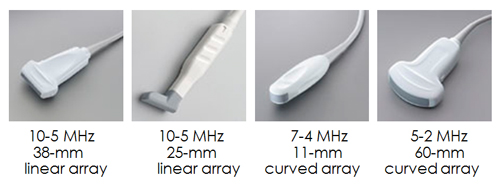
Examples of Philips Transducers:

(7-4 MHz Transducer)





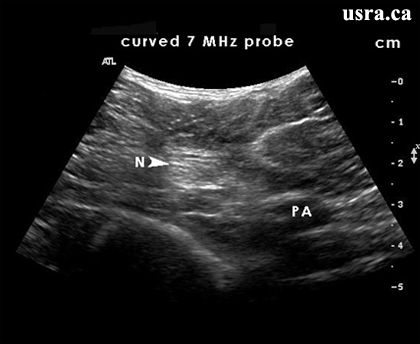
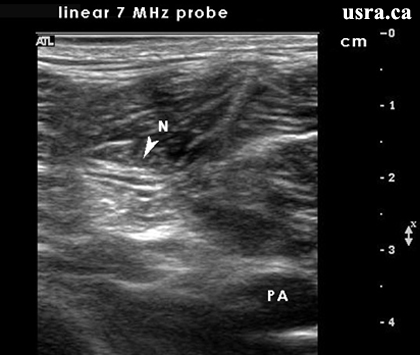
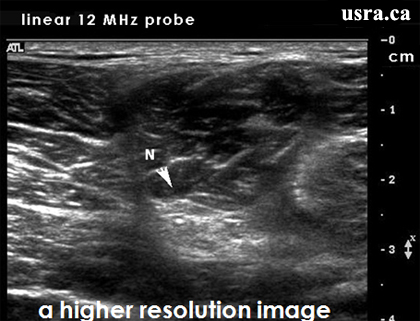

 Figure A shows a proper gain settings.
Figure A shows a proper gain settings.
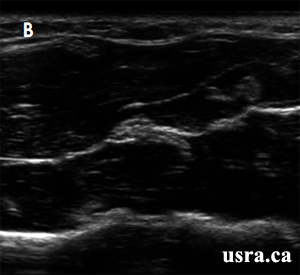 Figure B shows under gain thus the overall image is very dark. The muscle layers are not well visualized.
Figure B shows under gain thus the overall image is very dark. The muscle layers are not well visualized.
 Figure C shows excessive gain thus the overal image is very bright.
Figure C shows excessive gain thus the overal image is very bright.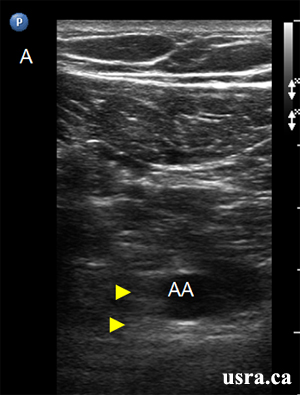 Figure A shows inappropriate focus setting at a superficial level (less than 2 cm) resulting in a dark image.
The target structures (AA = axillary vessels and Arrowheads = cords) are 5-6 cm deep to the skin.
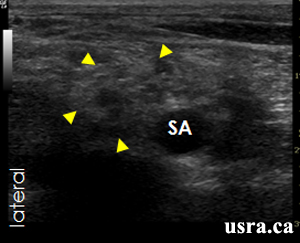
Figure A shows inappropriate focus setting at a superficial level (less than 2 cm) resulting in a dark image.
The target structures (AA = axillary vessels and Arrowheads = cords) are 5-6 cm deep to the skin.
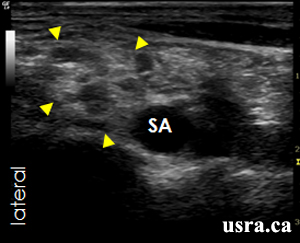
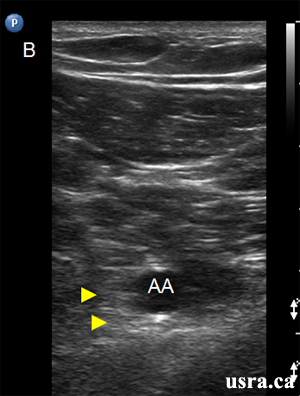 Figure B shows appropriate focus setting at 5-6 cm. The target structures (AA = axillary vessels and Arrowheads = cords) are 5-6 cm deep to the skin.
Figure B shows appropriate focus setting at 5-6 cm. The target structures (AA = axillary vessels and Arrowheads = cords) are 5-6 cm deep to the skin.