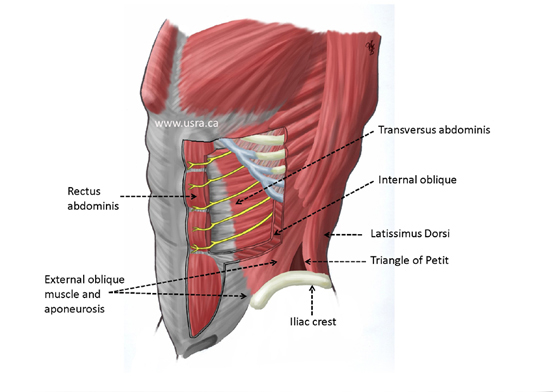
Anatomy
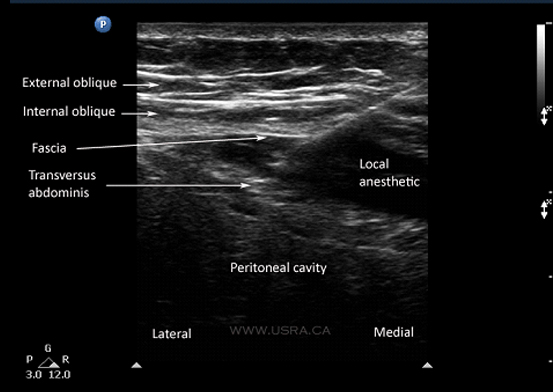
The anterior abdominal wall (skin, muscles, parietal peritoneum) is innervated
by the anterior rami of the lower 6 thoracic nerves (T7 to T12) and the first
lumbar nerve (L1). Terminal branches of these somatic nerves course through the
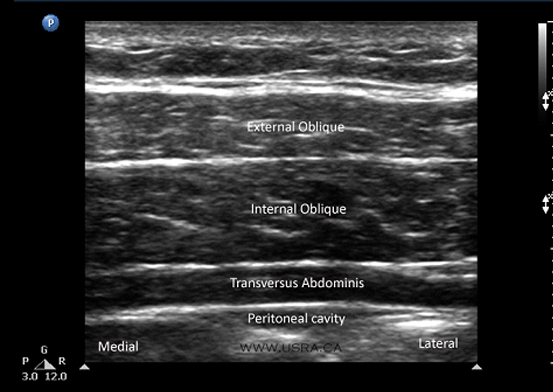
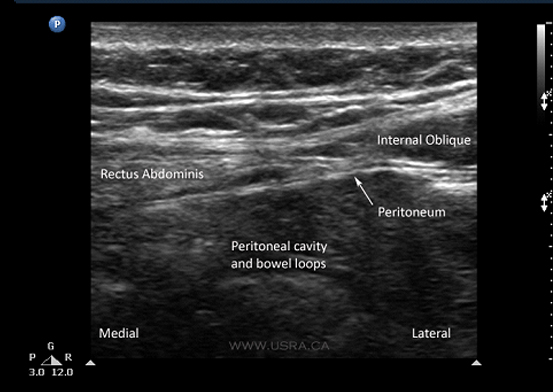
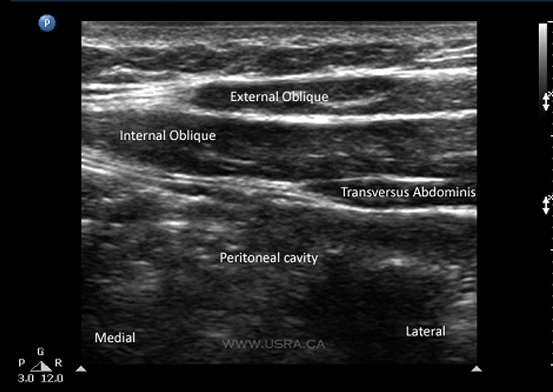
lateral abdominal wall within a plane between the internal oblique and transversus
abdominis muscles (Figure 1). This intermuscular plane is called the transversus
abdominis plane (TAP). Injection of local anesthetic within the TAP can therefore
potentially provide unilateral analgesia to the skin, muscles, and parietal
peritoneum of the anterior abdominal wall from T7 to L1.2
A recent cadaveric study of the TAP anatomy revealed the following points, which
are pertinent to performance of the TAP block.10
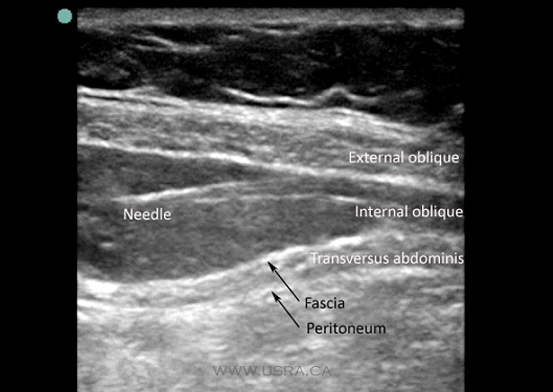
- There is a fascial sheath between the internal oblique and transversus abdominis muscles. The nerves lie deep to this fascia.
- Nerves of T6-T9 enter the TAP medial to the anterior axillary line. T6 enters the TAP just lateral to the linea alba, and T7-T9 at progressively increasing distances from the linea alba. Nerves running in the TAP lateral to the anterior axillary line,on the other hand, originate from segmental nerves T9-L1. This may explain the observation of some authors that the TAP block is only suitable for lower abdominal surgery.9,11
- There is extensive branching and communication of the segmental nerves in the TAP. In particular the T9-L1 branches form a so-called "TAP plexus" that runs with the deep circumflex iliac artery. This may partly account for the ability of a single injection to cover several segmental levels.
Figure 1 Anatomy of the transversus abdominis plane (TAP).