Scanning Technique
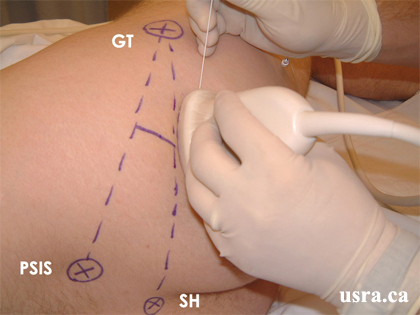
- Position the patient semi-prone (Sims' position) with the hip and knee flexed and the operative side uppermost.
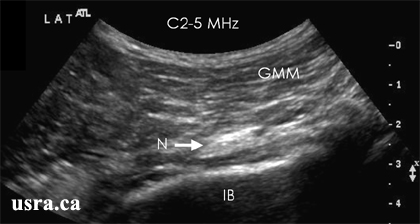
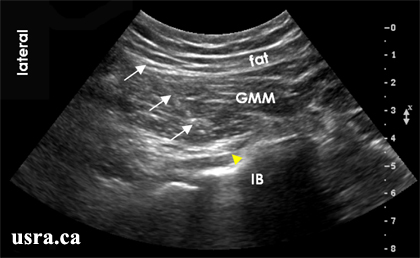
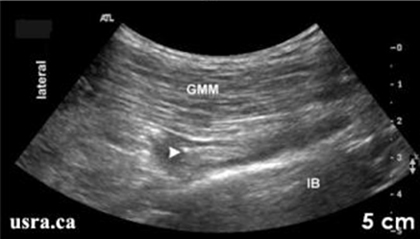
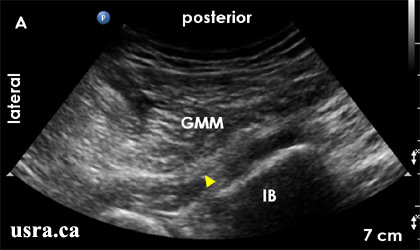
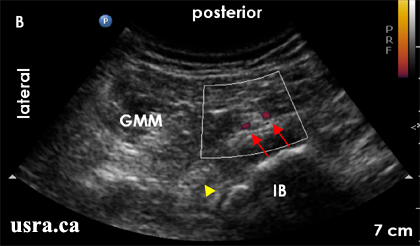
- After skin and transducer preparation (see transducer preparation section), place a curved low frequency 2-5 MHz transducer firmly on the buttock region to capture the best possible transverse view of the sciatic nerve.
- Optimize machine imaging capability. Select appropriate depth of field (usually > 4 cm from the skin surface), focus range and gain.
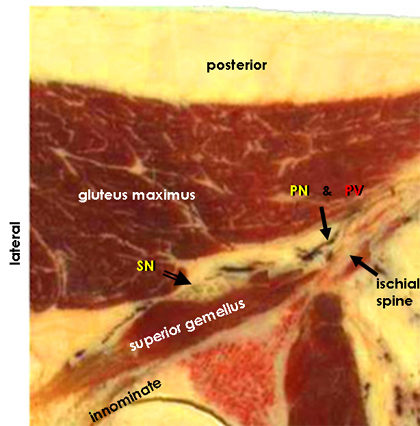
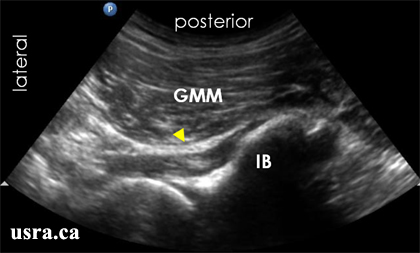
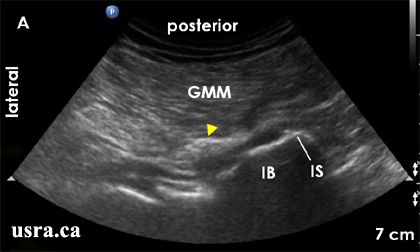
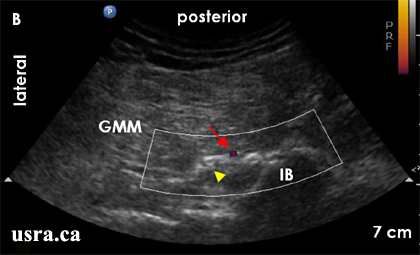
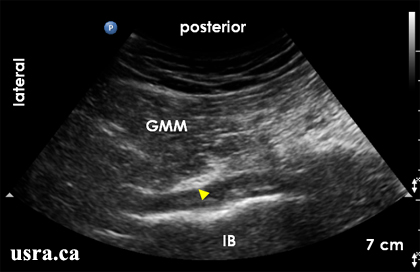
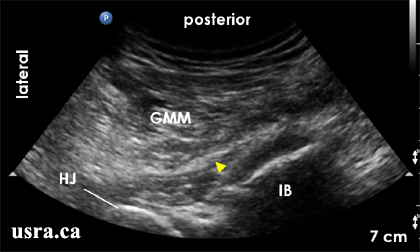
- Observe on the screen the transverse view of the sciatic nerve (short axis). The sciatic nerve in the gluteal region appears predominantly hyperechoic (bright) and is often wide and flat in the transverse view on ultrasound.
|
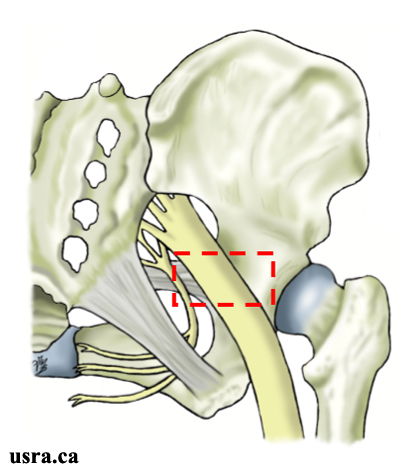
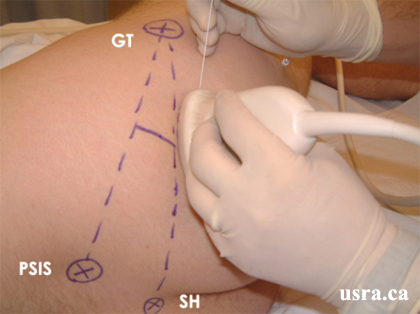
Transducer over right gluteal region. GT = greater trochanter PSIS = posterior inferior iliac spine SH = sacral hiatus |