Anatomy
The genitofemoral nerve (GFN), originating from L1 and L2 part of the lumbar plexus, is the smallest nerve of the plexus. After emerging from its origin, the GFN pierces the psoas major muscle at its ventral surface. The nerve may emerge as a single nerve or more often it is already divided into 1) the genital branch (gbGFN) and 2) the femoral branch (fbGFN). The gbGFN enters and courses within the inguinal canal (ICAN).
In males, the gbGFN is situated between the cremaster muscle and internal spermatic fasciae. The genital branch provides innervation to the cremaster muscle and the scrotal skin. Terminal sensory branches of the gbGFN may innervate part of the upper, inner, and medial thigh.
In females, the gbGFN provides sensation to the mons pubis and labia majora and the terminal sensory branches innervates part of the upper, inner, and medial thigh. The femoral branch provides innervation to the skin over the femoral triangle.
The inguinal canal is a cylindrical passage in the lower part of the anterior abdominal wall that runs obliquely anterior, inferior and medial (Figure 1). The inguinal canal is bounded by the aponeurosis of the external oblique muscle anteriorly (white arrows), the transversalis fascia posteriorly (purple arrows), the lower border of the transversus abdominis muscle cranially (brown arrows) and the inguinal ligament caudally (green arrow). Immediately outside and posterior to the inguinal canal is the inferior epigastric artery (IEA, red asterisk), a branch of the external iliac artery (EIA).
Figure 1. A parasagittal cross section of the lower abdominal wall showing the inguinal canal surrounded by arrows
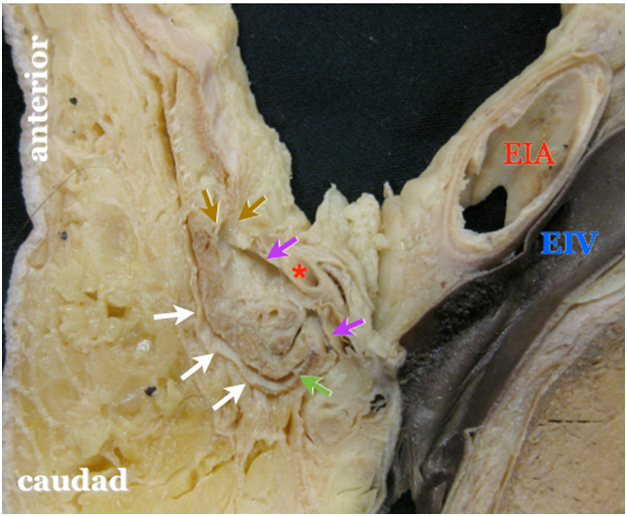 |
* = offspring of the inferior epigastric artery EIA = external iliac artery EIV = external iliac vein white arrow = aponeurosis of the external oblique muscle anteriorly purple arrow = transversalis fascia posteriorly brown arrow = lower border of the transversus abdominis muscle cranially green arrow = inguinal ligament caudally |
Movie 1. A parasagittal cross section of the inguinal canal
Inside the inguinal canal are 2 nerves, the genital branch of the genitofemoral nerve (gGbFN) and the ilioinguinal nerve (Figure 2). It also contains the spermatic cord in men with its three fascial layers and the round ligament of the uterus in women. The spermatic cord is enveloped by 3 fascial layers- the external spermatic fascia, the cremasteric fascia (CF) and the internal spermatic fascia (ISF). The gbGFN is inside the spermatic cord (usually in a duplication of the CF), while the ilioinguinal nerve runs inside the ICAN but outside the spermatic cord. Note that the ilioinguinal nerve is significantly larger in size than the gbGFN. Within the ISF are the vas deferens (with its small accompanying artery), the testicular artery, and the pampiniform venous plexus.
Figure 2A. Anatomy of the inguinal canal

The red box indicates the inguinal canal to be magnified.
Figure 2B. Magnification of the inguinal canal as outlined by the red box
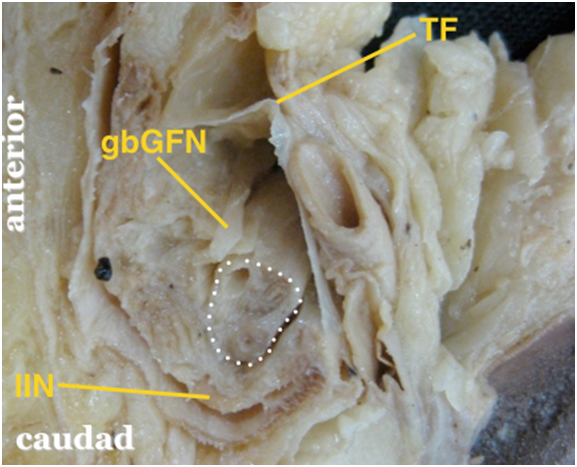 |
The white dotted area outlines the internal spermatic fascia of the spermatic cord containing the vas deferens, testicular artery and pampiniform plexus. gbGFN = genital branch of the genitofemoral nerve within the cremasteric facia (external spermatic fascia removed) IIN = ilioinguinal nerve which runs within the inguinal canal but outside the spermatic cord; note that the IIN is significantly bigger than the gbGFN TF = transversalis fascia |
Movie 2. Magnification of the inguinal canal

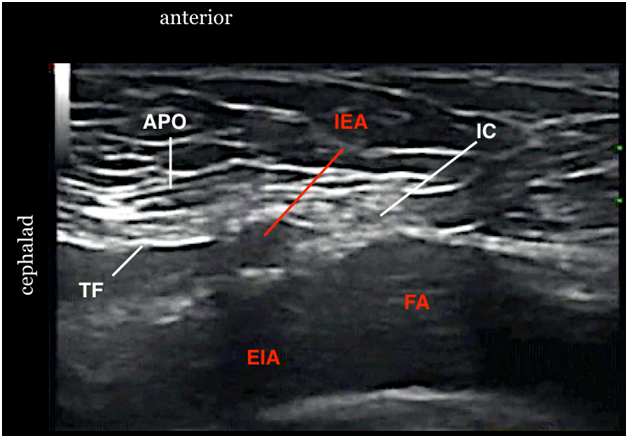

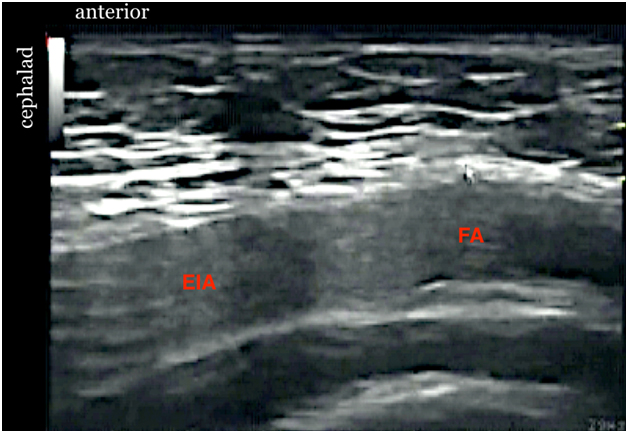
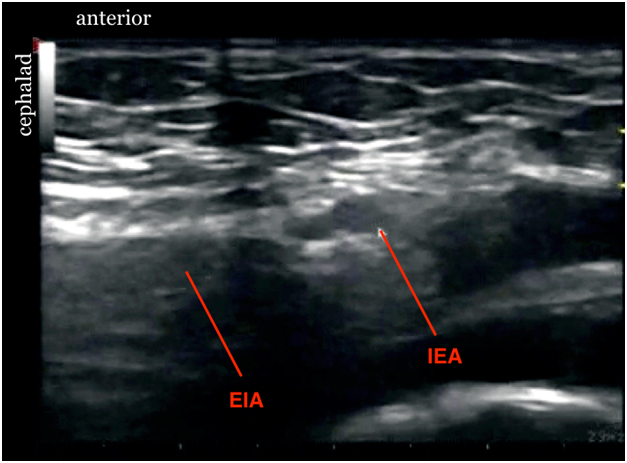
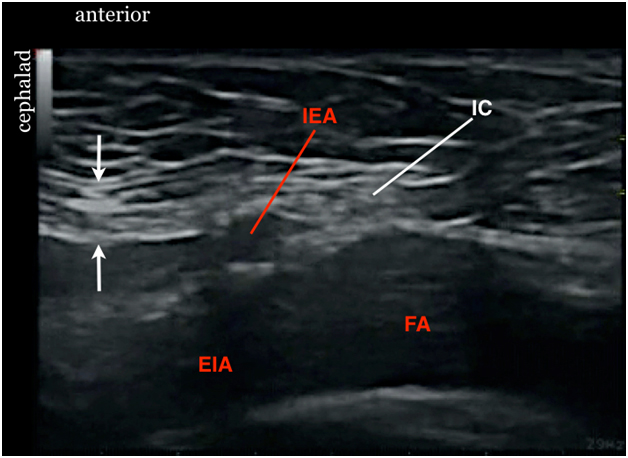

 Figure 10. Sonogram showing spermatic cord after injection
Figure 10. Sonogram showing spermatic cord after injection