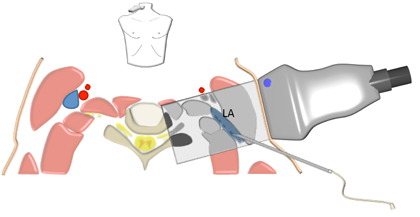
Anatomy The anterior spinal nerves of the cervical plexus emerge from the neural foramina of C1 to C4 in the lateral neck between the anterior and posterior tubercles of the respective transverse processes. They then pass along the lateral aspect of the longus colli and longus capitis muscles and the medial aspect of the levator scapulae and middle scalene muscles. Note that there is no anterior scalene muscle above the level of C4.
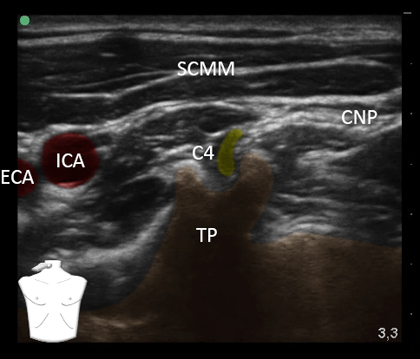
Transverse View of the Neck at the C4 Level Picture modified from the Visible Human Project Picture provided by Armbruster, Eichholz and Notheisen |
Schematic Illustration of Key Anatomical Structures at the C4 Level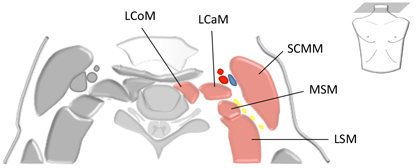 LCaM = Longus capitis muscle LCoM = Longus colli muscle LSM = Levator scapulae muscle MSM = Middle scalene muscle SCMM = Sternocleidomastoid muscle Picture provided by Armbruster, Eichholz and Notheisen |
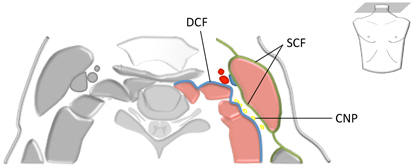
The nerves of the cervical plexus run through the deep cervical fascia and enter the "Cervical Nerves Pathway" (CNP)
which is the space between the deep cervical fascia (covering the paravertebral muscles) and the superficial cervical
fascia (covering the sternocleidomastoid muscle)
Schematic Illustration of the Deep and Superficial Fascia of the Neck
|
CNP = Cervical nerves pathway DCF = Deep cervical fascia SCF = Superficial cervical fascia Picture provided by Armbruster, Eichholz and Notheisen |
Nerves of the cervical plexus pass from medial to lateral underneath the sternocleidomastoid muscle,
and pierce the superficial cervical fascia at the lateral edge, corresponding to Erb's point.
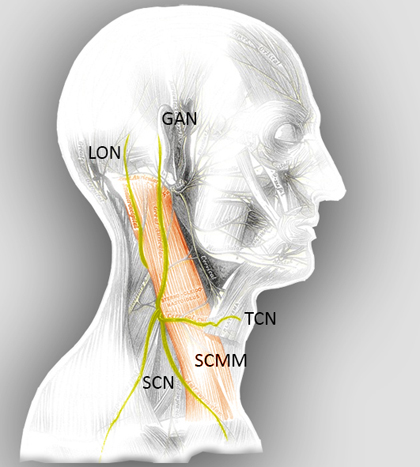
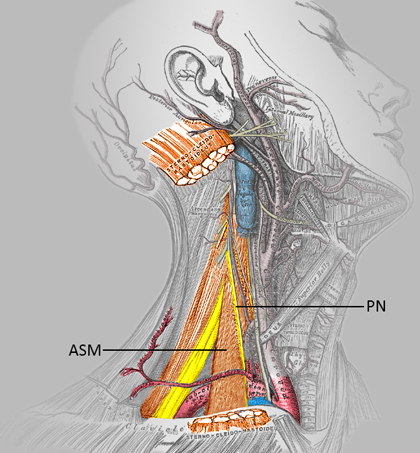
As shown in the figure below, cutaneous branches that come off the cervical plexus are:
1. |
the lesser occipital nerve, |
2. |
the great auricular nerve, |
3. |
the transverse cervical nerve and |
4. |
the supraclavicular nerve |
Cutaneous branches of the cervical plexus provide sensory innervation to the skin of the anterolateral
neck, the surrounding muscles and connective tissue.
Muscular branches of the cervical plexus are:
- the phrenic nerve, from C3 to C5 (primarily C4), innervates the diaphragm and pericardium
- ansa cervicalis innervates chin muscles above the hyoid bone and strap muscles of the neck below
- branches to the anterior and middle scalene muscles
It is important to note that the vagal nerve (X), the glossopharyngeal nerve (IX) and
sensory branches of sympathetic nerves (from superior cervical ganglion) provide sensory
innervation to the intima of the carotid artery and the glomus organ.
Thus blockade of the cervical plexus only provides sensory anesthesia to the lateral
neck, but not to the carotid artery and glomus organ. For carotid endarterectomy surgery,
it is necessary to instill local anesthetic in the carotid sinus region to prevent
bradycardia independent of the cervical plexus block.
Superficial Cutaneous Branches of the Cervical Plexus
|
GAN = Great auricular nerve LON = Lesser occipital nerve SCMM = Sternocleidomastoid muscle SCN = Supraclavicular nerves TCN = Transverse cervical nerve Picture modified from Grays Anatomy Picture provided by Armbruster, Eichholz and Notheisen |





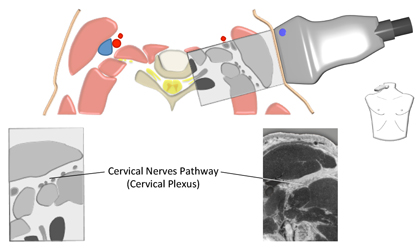
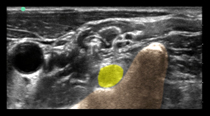
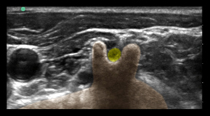
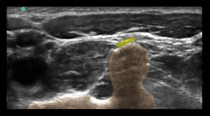
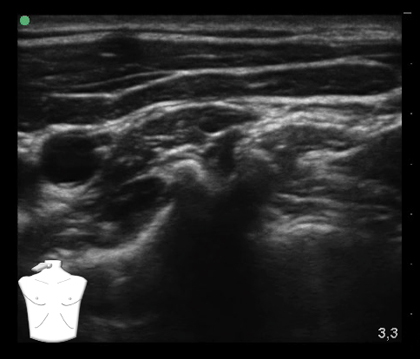 Picture provided by Armbruster, Eichholz and Notheisen
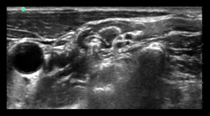
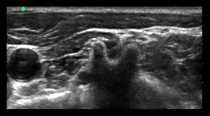
Picture provided by Armbruster, Eichholz and Notheisen
 C4 = Spinal nerve C4
C4 = Spinal nerve C4

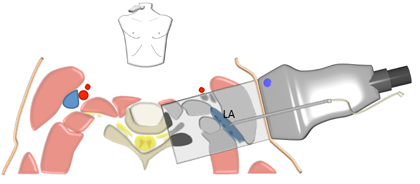
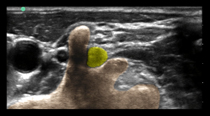
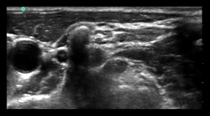
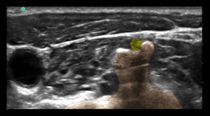
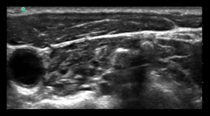
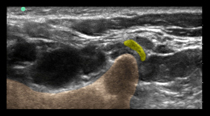
 Picture provided by Armbruster, Eichholz and Notheisen
Picture provided by Armbruster, Eichholz and Notheisen
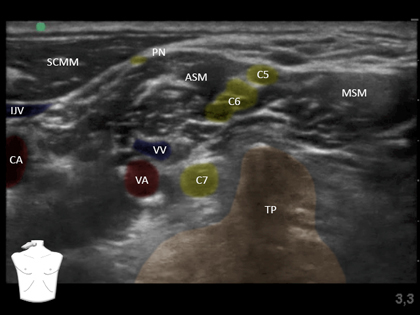 C5 = Nerve root C5
C5 = Nerve root C5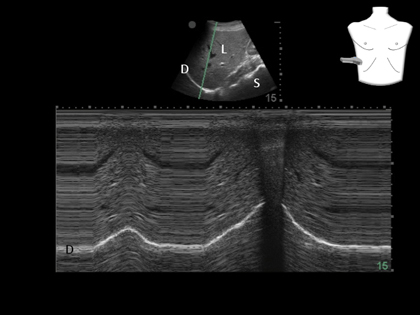 D = Diaphragm
D = Diaphragm 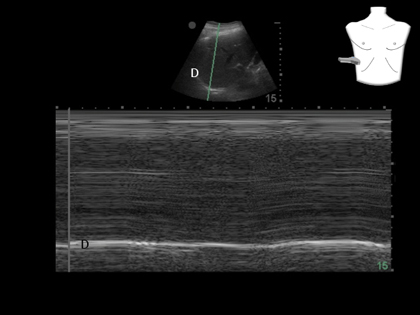 D = Diaphragm
D = Diaphragm