Scanning Technique
- Position the patient prone and keep the toes off the bed if electrical stimulation will be used to evoke foot movement.
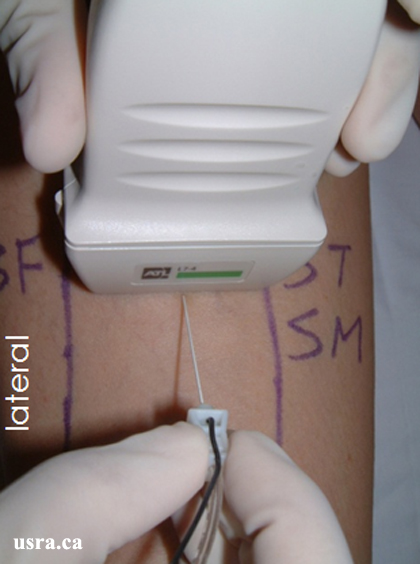
- After skin and transducer preparation, place a linear 38 mm, 7-10 MHz transducer in a transverse plane above the popliteal crease.

|
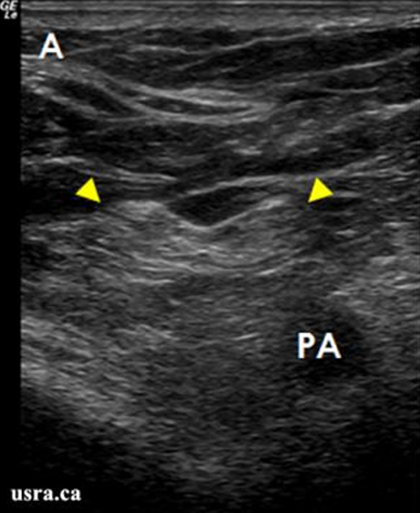
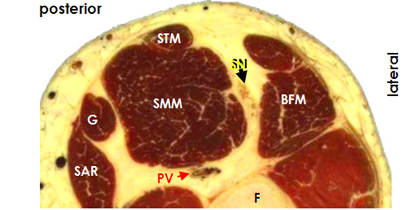
BF = biceps femoris muscle SM = semimembranosus ST = semitendinosus muscle |

|
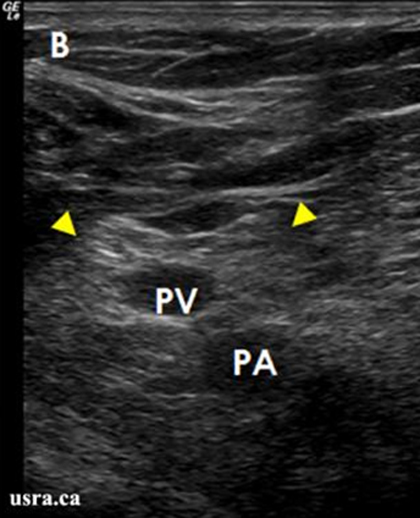
BF = biceps femoris muscle SM = semimembranosus ST = semitendinosus muscle |
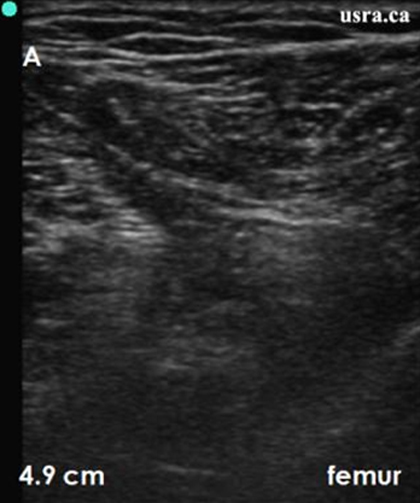
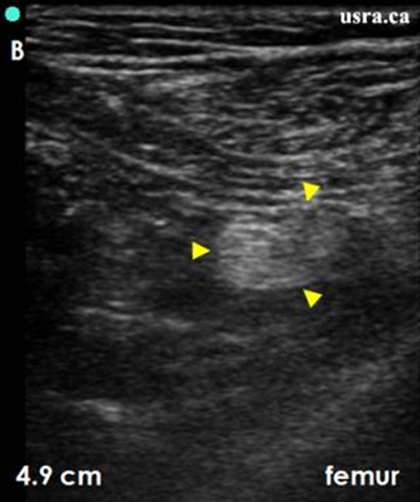
- Optimize machine imaging capability. Select the appropriate depth of field (usually within 5 cm), focus range (usually within 2-3 cm) and gain.
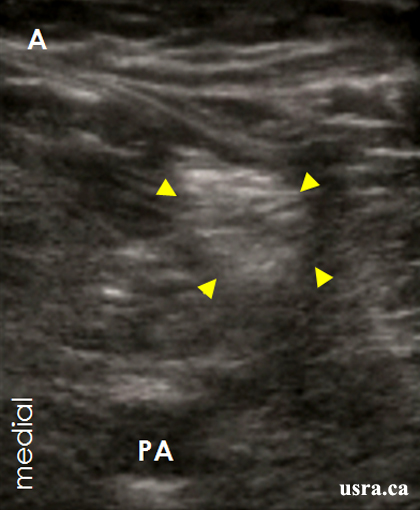
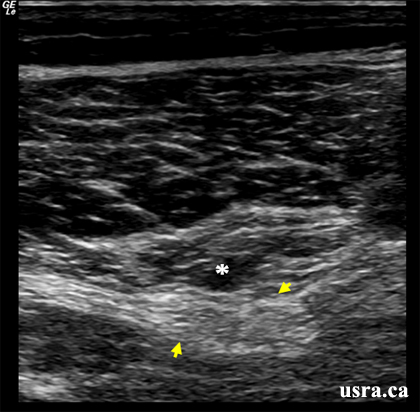
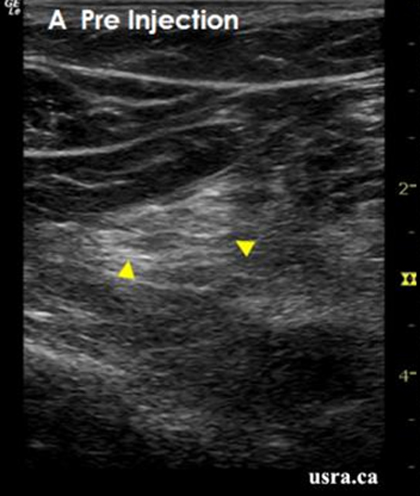
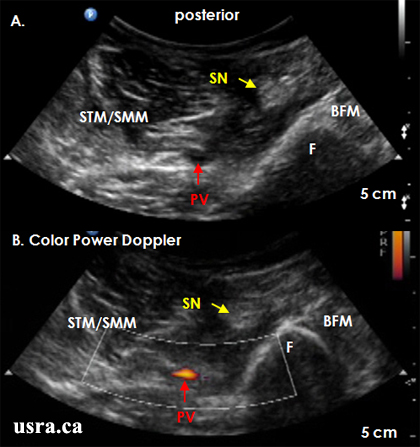
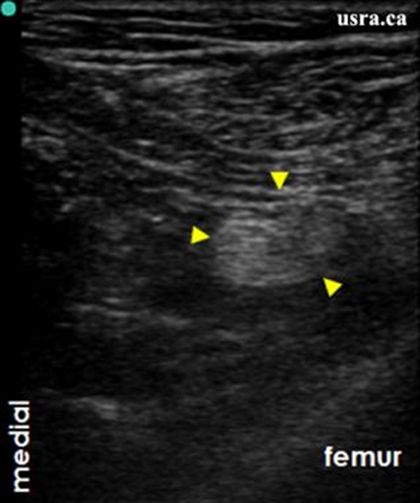
- Obtain a transverse view of the sciatic nerve.
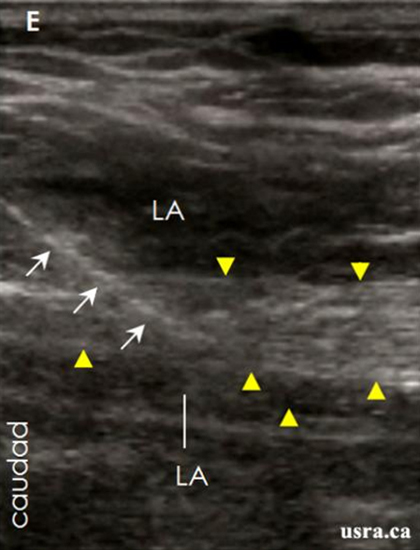
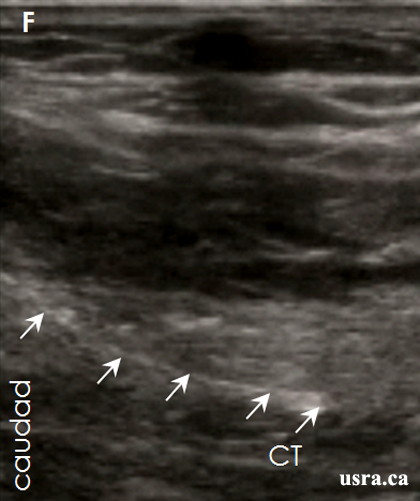
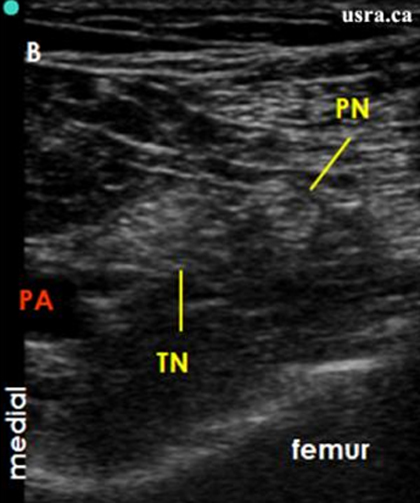
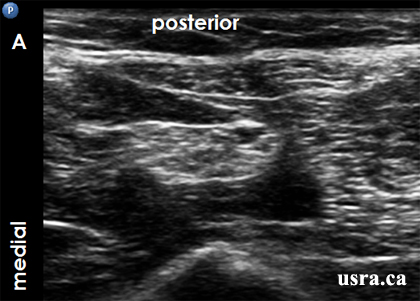
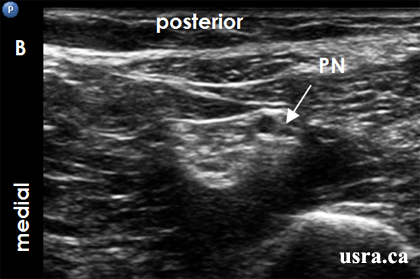
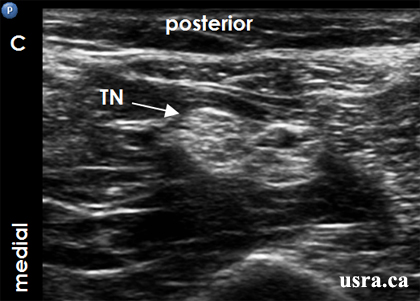
- Scan the region proximally and distally to assess nerve anatomy and the point at which the sciatic nerve branches into its tibial and peroneal components.
- Aim to block the sciatic nerve before it divides.
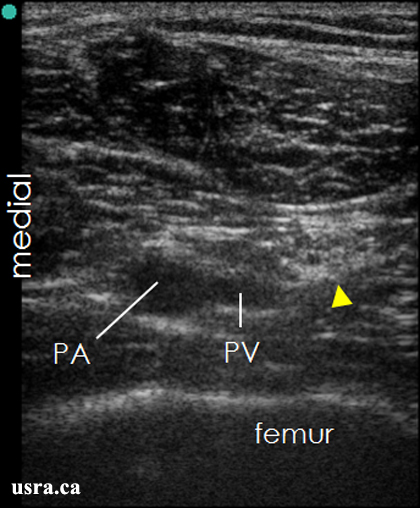
- The sciatic nerve is commonly hyperechoic in this region and is found lateral to the popliteal artery. It is often necessary to angle the transducer caudally to enhance nerve visibility.


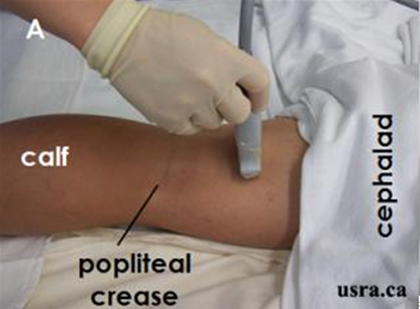


 A. Patient preparation, sterile draping and pre-block scanning
A. Patient preparation, sterile draping and pre-block scanning
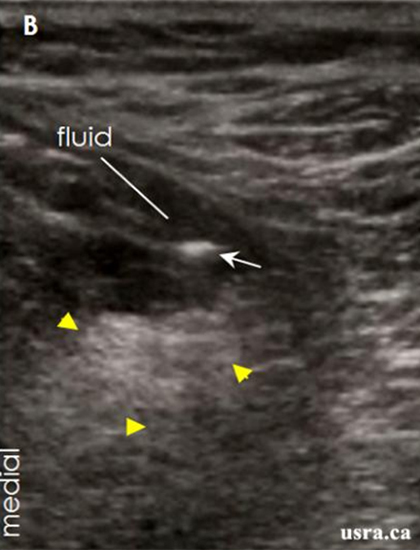
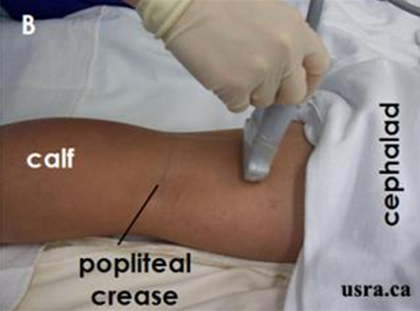
 B. Out of plane needle advancement under ultrasound guidance
B. Out of plane needle advancement under ultrasound guidance
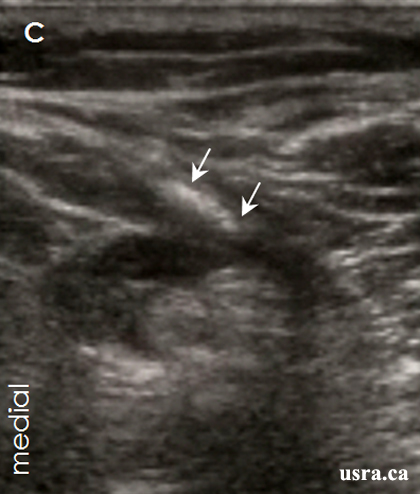
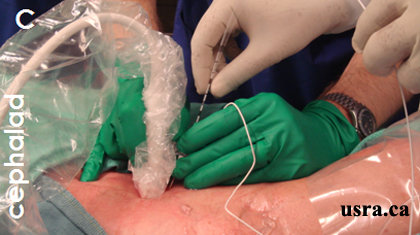 C. Catheter insertion with the help of an assistant
C. Catheter insertion with the help of an assistant
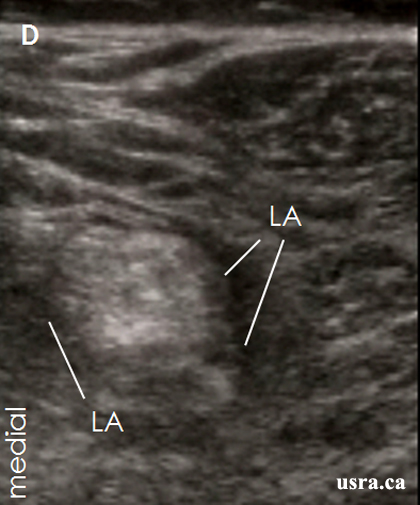
 D. Catheter exits in the distal 1/3 part of the thigh
D. Catheter exits in the distal 1/3 part of the thigh
 E. Catheter is secured with dermabond at the exit site
E. Catheter is secured with dermabond at the exit site
 F. Catheter is further secured with a transparent dressing
F. Catheter is further secured with a transparent dressing