Scanning Technique
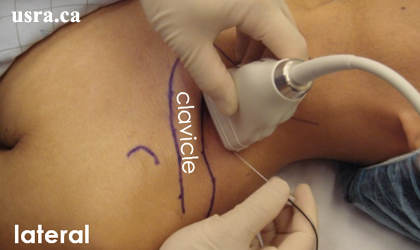
- After skin and transducer preparation (see transducer preparation section), place a linear 38-mm, high frequency 10-15 MHz transducer firmly over the supraclavicular fossa in the coronal oblique plane to obtain the best possible transverse view of the subclavian artery and brachial plexus.
- Position the patient supine with the head slightly turned to the contralateral side.

|
Transducer over left supraclavicular fossa |
- Optimize machine imaging capability by selecting the appropriate depth of field (within 2-3 cm), focus range and gain.
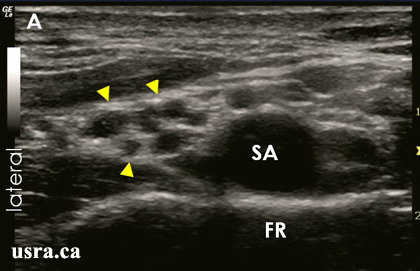
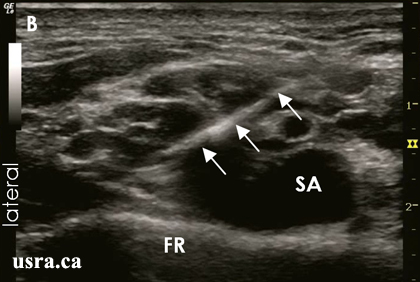
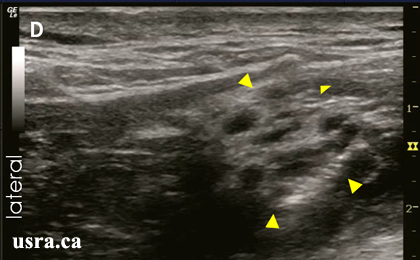
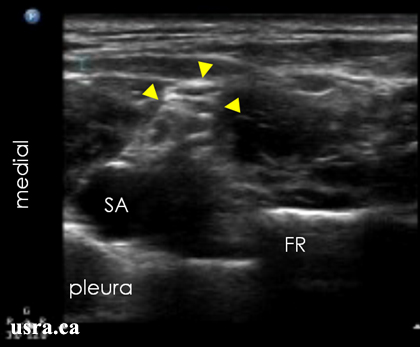
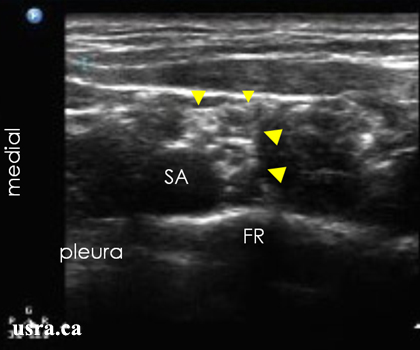
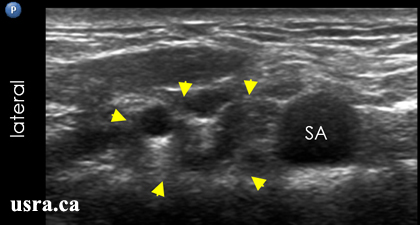
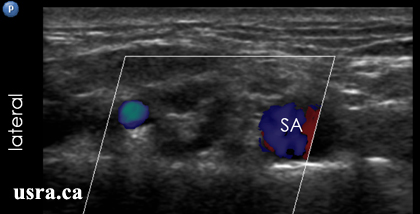
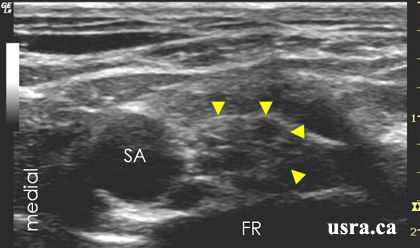
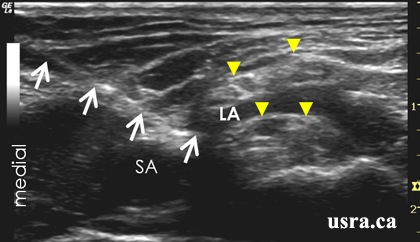
- Visualize the trunks or divisions in the transverse view (short axis). Nerves in the supraclavicular region appear hypoechoic and are round or oval. The brachial plexus is located lateral and posterior to the pulsatile subclavian artery and superior to the first rib.

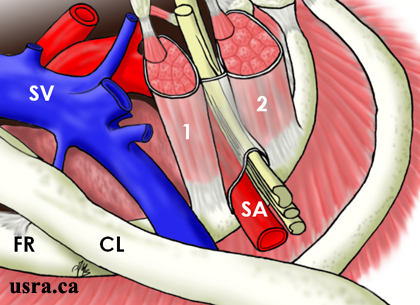
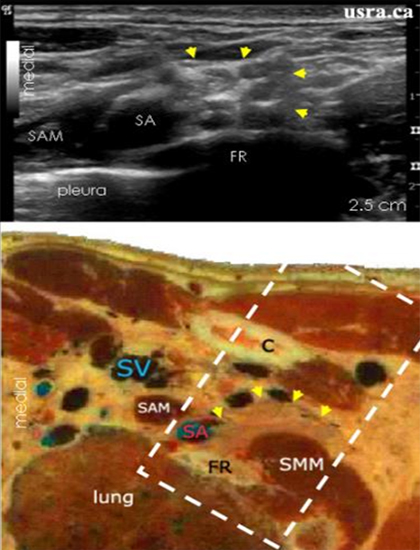

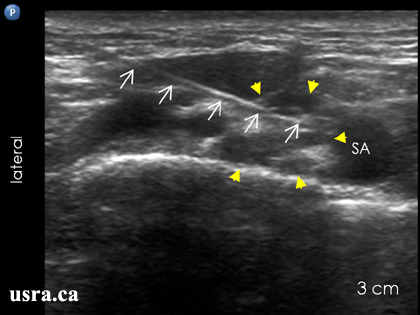
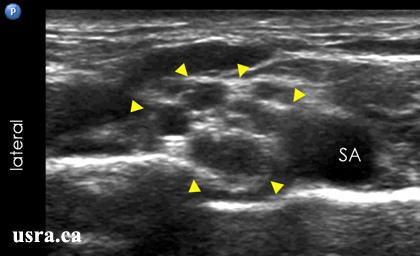
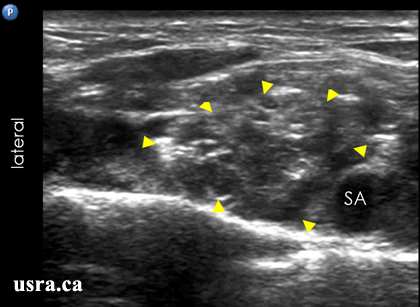

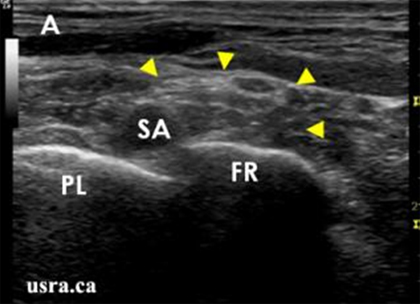 Figure A shows transducer in proper position. The structures of interest are clearly visualized.
Figure A shows transducer in proper position. The structures of interest are clearly visualized.

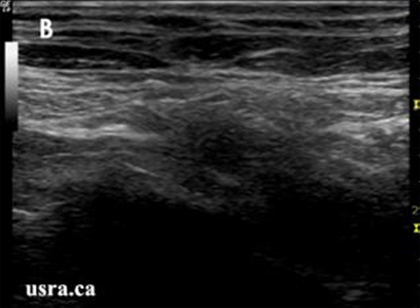

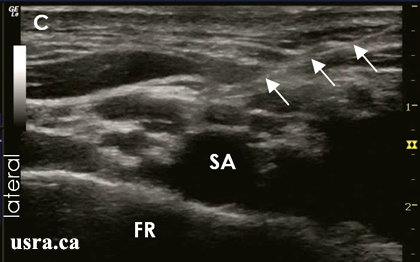
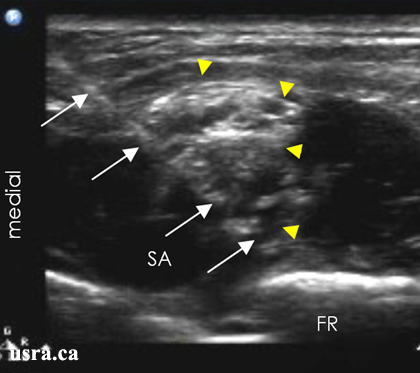
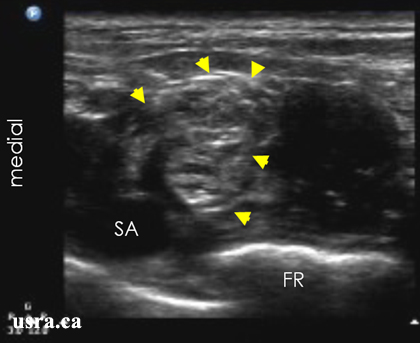
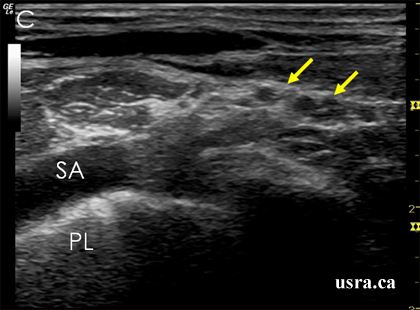 Figure C shows that the transducer is angled too posteriorly. The
subclavian artery and the brachial plexus are now visualized oblique and the
view is not optimal.
Figure C shows that the transducer is angled too posteriorly. The
subclavian artery and the brachial plexus are now visualized oblique and the
view is not optimal.

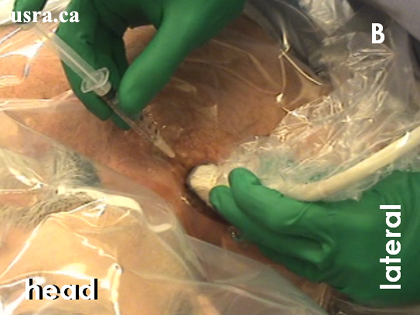
 A. Patient preparation and sterile draping
A. Patient preparation and sterile draping
 B. Pre-block scanning and local anesthetic skin infiltration
B. Pre-block scanning and local anesthetic skin infiltration
 C. Block needle advancement (medial to lateral) under ultrasound guidance
C. Block needle advancement (medial to lateral) under ultrasound guidance
 D. Catheter insertion with the help of an assistant
D. Catheter insertion with the help of an assistant
 E. Removal of block needle
E. Removal of block needle
 F. Catheter exits above the clavicle
F. Catheter exits above the clavicle