Scanning Technique
- Position the patient supine and abduct the arm to approximately 90 degrees.
- After skin and transducer preparation (see transducer preparation section), place a linear 38-mm, high frequency 10-12 MHz transducer firmly on the upper 1/3 of the arm to capture the best possible transverse view of the nerves in the midhumeral region.

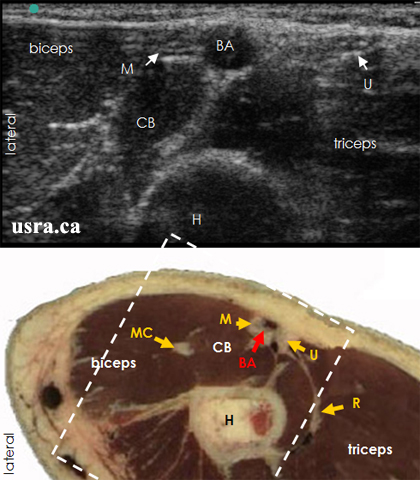
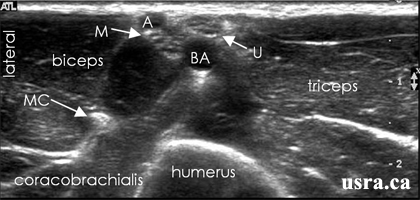
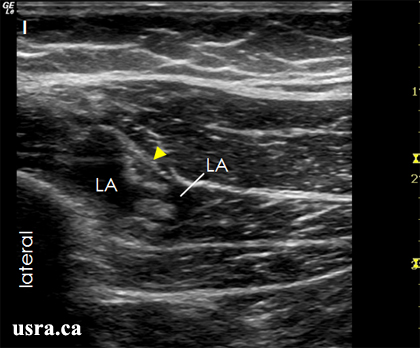
Transducer over left midhumeral region (upper 1/3 of the arm).
- Optimize machine imaging capability by selecting the appropriate depth of field (within 1-2 cm), focus range (usually within 1 cm) and gain.
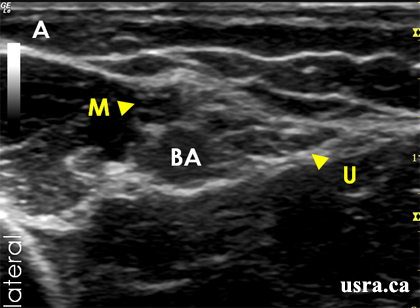
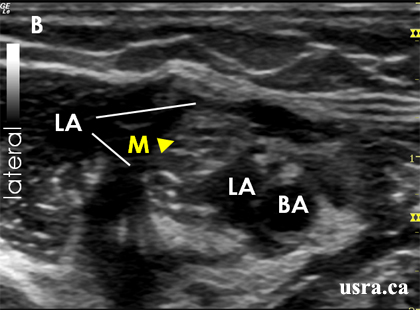
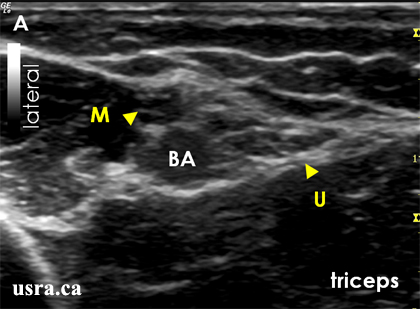
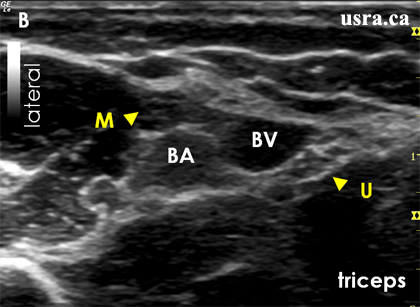
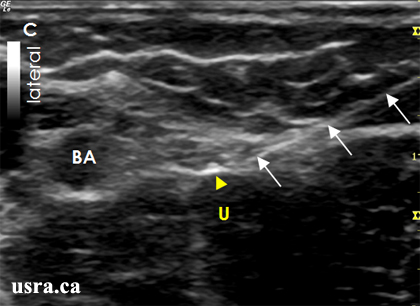
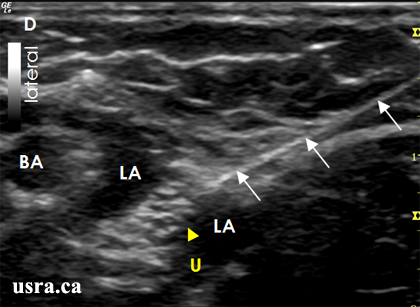
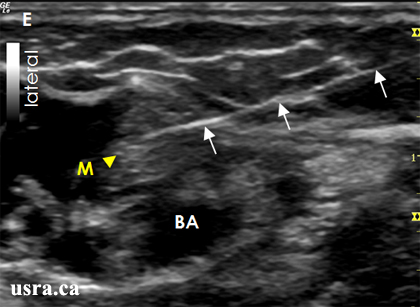
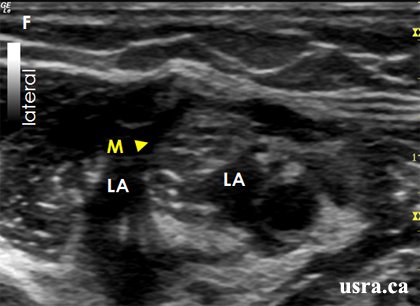
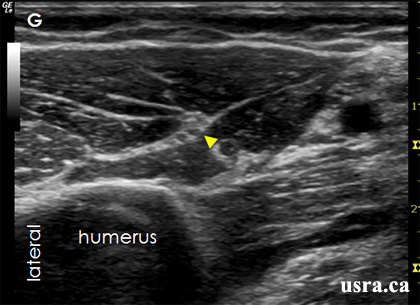
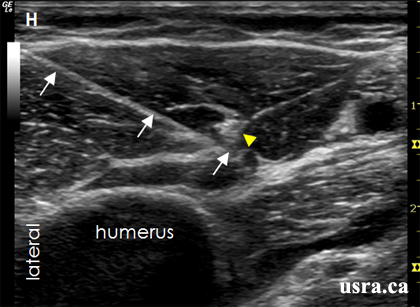
- Visualize the median, ulnar, and musculocutaneous nerves in transverse view (short axis). Nerves in the midhumeral region have mixed echogenicity (honeycomb appearance with a mixture of hypoechoic nerve fascicles and hyperechoic connective tissues). The nerves are round or oval, and are located next to the brachial artery and vein.