Anatomy
The Third Occipital Nerve (TON)
The C3 dorsal ramus has both a medial and a lateral portion and furthermore, the medial portion has a superficial and a deep segment. From an anatomical perspective, the TON is simply the big superficial part (or branch) of the medial portion of the C3 dorsal ramus. This part is also called the least occipital nerve. In clinical use, however, the whole C3 dorsal ramus itself is often called the TON.
After emerging from the spinal nerve, the C3 dorsal ramus courses posteriorly, medial to the posterior intertransverse muscles, and then crosses over the lateral aspect of the C2/C3 facet joint. The TON gives off the only sensory branches to the C2/C3 facet joint.
The nerve courses further dorso-medially and cephalad to pierce and supply both the semispinalis and splenius capitis muscles at the C2 (axis) level. It continues to travel cephalad and emerges superficial by piercing the trapezius muscle at the C1 (atlas) level. At its final destination, the occiput level, the TON provides sensory innervation to a small area of skin just below the superior nuchal line.
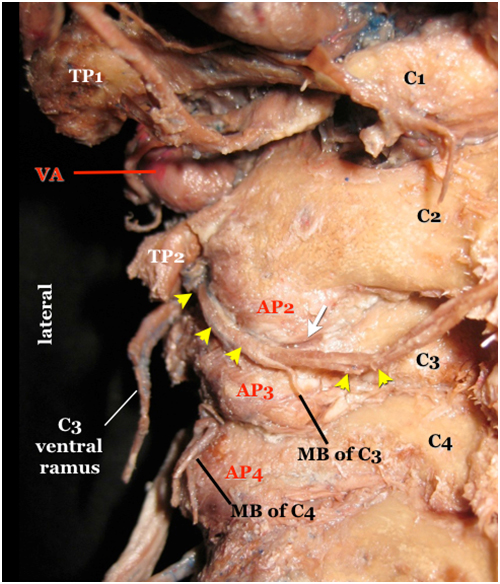
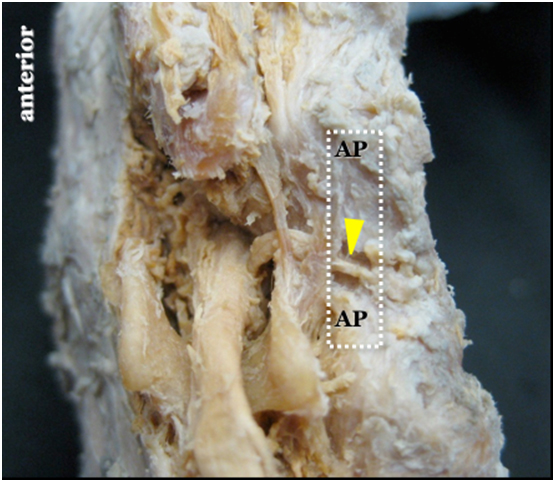
In Figure 1, note that the TON (arrowheads) first appears caudad to the transverse process of axis (TP2) before reaching the surface of the C2/C3 facet joint gap over its lateral aspect. The white arrow indicates the posterior C2/C3 joint gap.
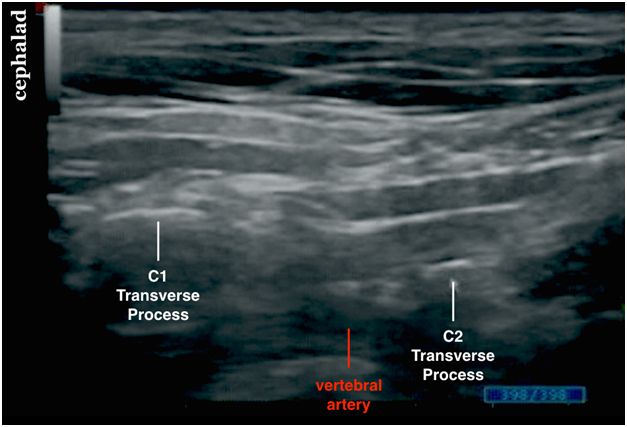
Figure 1 shows a number of important internal anatomical landmarks for localization of the third occipital nerve.
They are:
- the C1 and C2 transverse processes (bony landmarks);
- the typical wavy appearance of the lateral aspects of articular pillars of cervical vertebrae (bony landmarks; see ultrasound image); and
- the vertebral artery (a vascular landmark) in between the C1/C2 transverse processes.
- The Cervical Medial Branches (C-MB)
Figure 1. A posterior view of the cervical spine showing the third occipital nerve in a cadaver specimen
|
arrowheads = TON; first appears caudad to the transverse process of axis (TP2) before reaching the surface of the C2/C3 facet joint gap over its lateral aspect. AP = articular process C1 = atlas, posterior arch C2 = axis, lamina MB = medial branch VA = a segment of the vertebral artery appearing between the transverse process of axis (TP2) and the transverse process of atlas (TP1) white arrow = the posterior C2/C3 joint gap |
Movie 1. TON and cervical medial branch anatomy
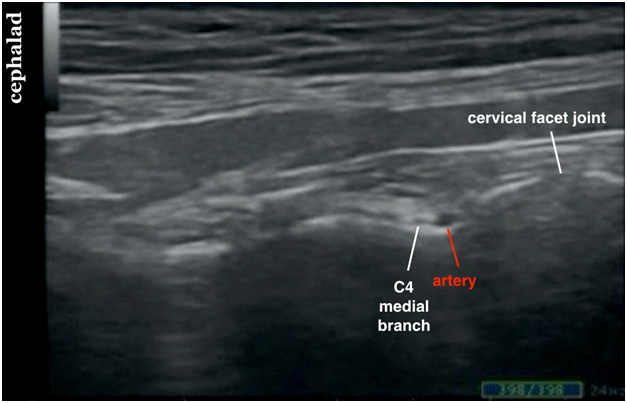
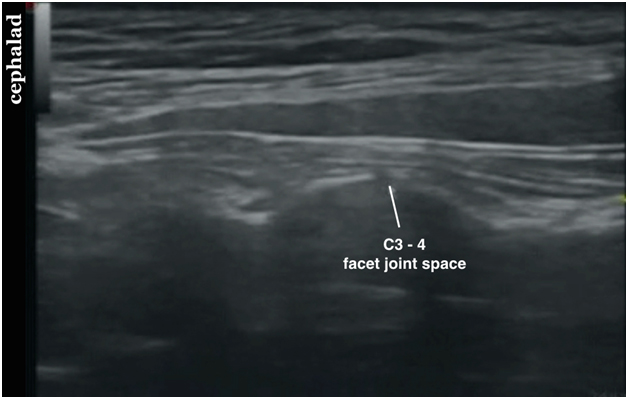
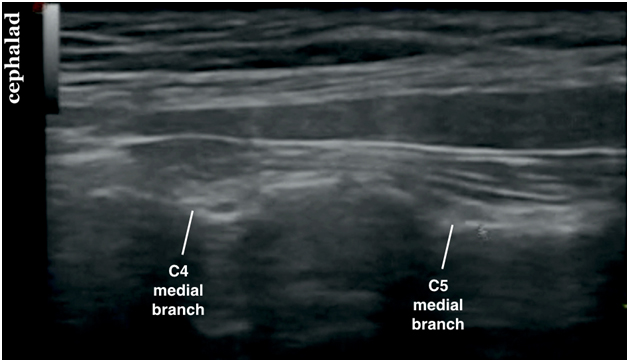
The deep medial branch of C3 dorsal ramus and medial branches of C4-C7 dorsal rami innervate the cervical facet joints. It is important to realize that each facet joint from C3/C4 and below receives innervation from one medial branch above and one below.
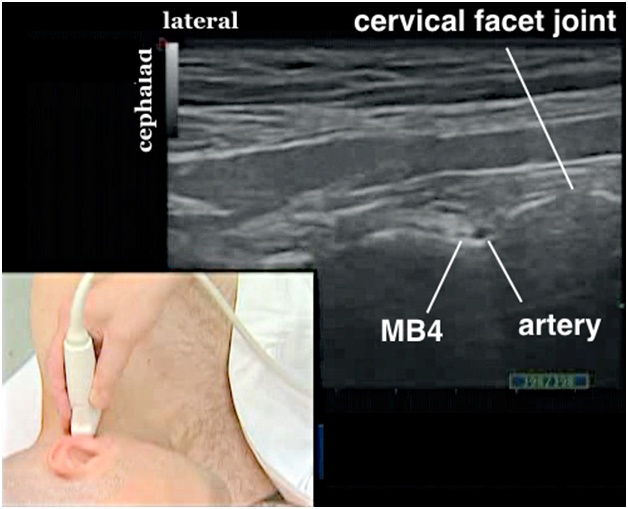
The cervical medial branches are smaller in caliber than the TON. The medial branches emerge from the respective dorsal ramus of a spinal nerve, and each dorsal ramus is held in place by the tendinous parts of the erector spinae muscles. Each cervical medial branch then courses around the waist between the articular processes. For example, the medial branch of C4 is seen within the waist of the superior and inferior articular processes of C4 (Figure 2). The medial branches get progressively smaller at lower cervical levels.
Note that the C4 medial branch (yellow arrowhead in Figure 2) arising from the C4 dorsal ramus (green arrowhead) is held in place by the tendon slips (asterisk) of the erector spinae muscles. The C4 medial branch is located within the waist of the articular process (AP) of C4 cervical vertebra.
Figure 2. Cadaver dissection showing the C4 medial branch
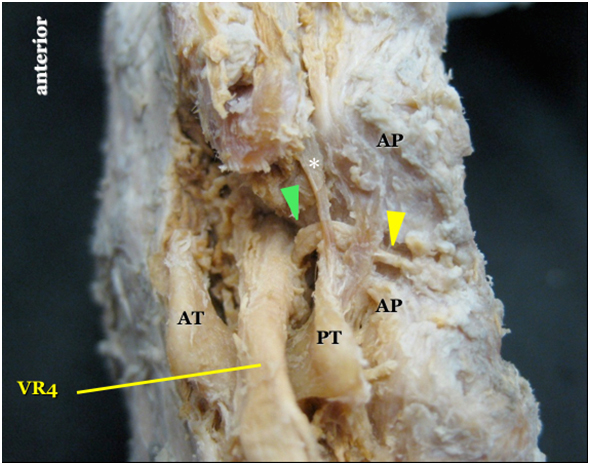
|
yellow arrowhead = C4 medial branch green arrowhead = C4 dorsal ramus * = tendon slip of the erector spinae muscle AP = articular processes of C4 AT = anterior tubercle of C4 transverse process PT = posterior tubercle of C4 transverse process VR4 = the C4 ventral ramus |
Movie 2. Cervical medial branch anatomy

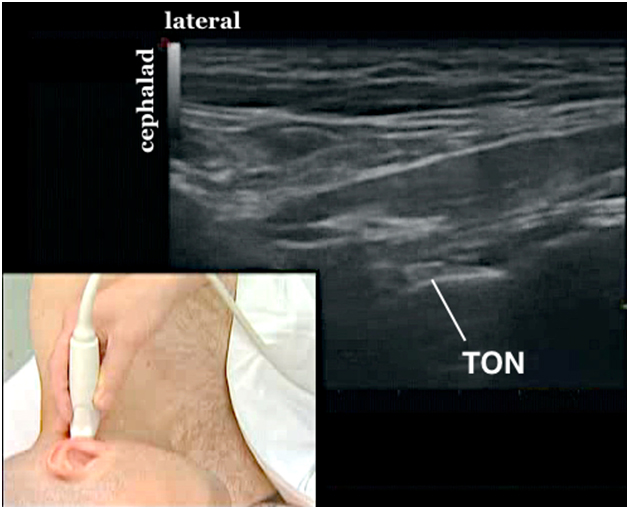

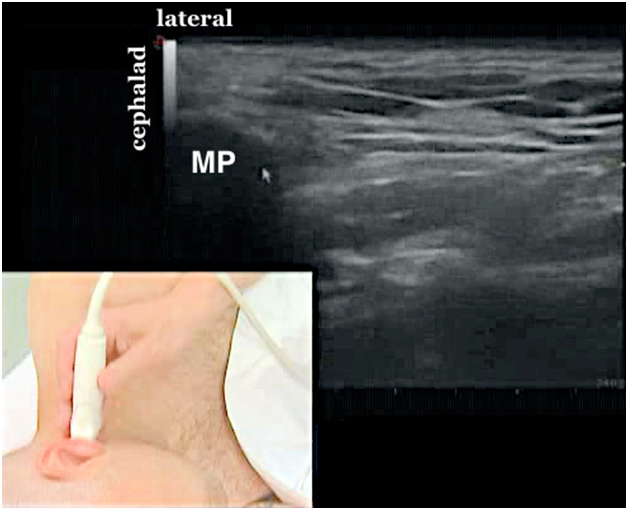
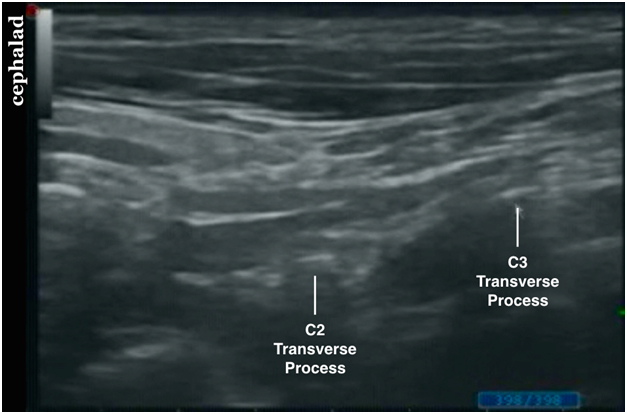
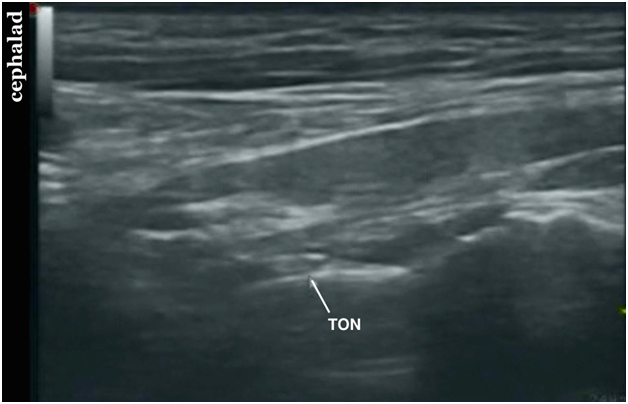
 After a systematic anatomical survey and locating the C1, C2 and C3 transverse processes and their corresponding facet joints, identify the TON over the C2/C3 facet joints.
Using the hydrolocation technique with saline, insert a 5 cm short bevel 24 G needle out-of?plane to approach the TON in the anterior to posterior direction (Figure 14).
Aim to see distention of the space surrounding the TON and lifting up of the hyperechoic tissue plane (the tendinous part of the erector spinae muscle) at the time of hydrodissection.
After a systematic anatomical survey and locating the C1, C2 and C3 transverse processes and their corresponding facet joints, identify the TON over the C2/C3 facet joints.
Using the hydrolocation technique with saline, insert a 5 cm short bevel 24 G needle out-of?plane to approach the TON in the anterior to posterior direction (Figure 14).
Aim to see distention of the space surrounding the TON and lifting up of the hyperechoic tissue plane (the tendinous part of the erector spinae muscle) at the time of hydrodissection.