|
Dr. Jens Børglum
Associate Professor, Consultant, Head of Research
Zealand University Hospital, Copenhagen University
Denmark
Biosketch
Biosketch

|
Dr. Jens Børglum
Associate Professor, Consultant, Head of Research
Zealand University Hospital, Copenhagen University
Denmark
|
Jens Børglum was educated at Aarhus University, Denmark.
Medical doctor in 1990. Studies for PhD thesis were conducted
at Centre de Biochemie, Universite de Nice-Sophia Antipolis,
France and at Aarhus University Hospital, Denmark. PhD 1997.
MBA(ex) 2002 (Henley Management Collage, London, UK). Currently
employed as Consultant Anaesthetist, Associated Professor,
Head of Research, PhD, Zealand University Hospital, Copenhagen
University, Denmark. Jens Børglum has published more
than 70 articles and book chapters predominantly in
international peer-reviewed journals. Since 2010 Jens
Børglum has been invited as speaker and member of the
scientific faculty to more than 60 international congresses
and meetings all over the world: ESRA, ASRA, ISURA, NYSORA,
ISSPS, ASURA, ASA. Main interest: Ultrasound guided
peripheral nerve blocks; i.e. SPEDI block, SSPS block,
PSPS block, Shamrock lumbar plexus block, BD-TAP block,
TQL block, pudendal nerve block, suprascapular continuous
nerve block, PSP block, and femoral triangle block.
×
|
 |
Dr. Bernhard Moriggl
Professor, Division of Clinical and Functional Anatomy Department of Anatomy Histology and Embryology
Innsbruck Medical University
Innsbruck, Austria
Biosketch
Biosketch

|
Dr. Bernhard Moriggl
Professor, Division of Clinical and Functional Anatomy Department of Anatomy Histology and Embryology
Innsbruck Medical University
Innsbruck, Austria
|
Professor Moriggl started his University career in 1986 in Innsbruck and has done ultrasonography ever since. Some of Prof. Moriggl's former scholars are practically concerned with ultrasonography. He often serves as mentor and senior author to them. Prof. Moriggl has had clinical training, especially in diagnostic imaging. This practical background was the starting point of his constantly increasing engagement in regional anesthesia and pain medicine. In 2008 he has become one of the founding members of a Special Interest Group (SIG) for Ultrasound in Pain Medicine (USPM) within the ASRA and is now its educational director. Prof. Moriggl is a contributor of the Practical Guide by Vincent Chan as well as to the pocket-book on Principals and Practical Implementation by Peter Marhofer. He was author of the chapter: "Spine Anatomy and Sonoanatomy for pain physicians" within the Atlas of Ultrasound-Guided Procedures in Interventional Pain Management, released in January 2011. The second edition will be released in autumn 2015 which include a brand new chapter on the "GON" (done together with Manfred Greher from Vienna). Prof. Moriggl has plenty of international cooperation both practically and scientifically. The most recent example of the former is co-development and support of the WAAPMU (World Academy of Pain Medicine Ultrasonography) and the one for the latter is joining Jens Børglum and Thomas Fichtner Bendtsen from Copenhagen in Denmark.
×
|
 |
Dr. Thomas F. Bendtsen
Associate Professor Consultant
Aarhus University Hospital, Aarhus
Denmark
Biosketch
Biosketch

|
Dr. Thomas F. Bendtsen
Associate Professor Consultant
Aarhus University Hospital, Aarhus
Denmark
|
Dr. Bendtsen is a research anesthetist at Aarhus University Hospital and Associate Professor affiliated to the Faculty of Health at Aarhus University, Denmark, where he obtained the gold medal of the university for a prize dissertation and the PhD degree. His main research interests are ultrasound guided regional anaesthesia and analgesia especially lumbosacral plexus blocks, lower limb blocks and real time image fusion of ultrasound and MRI. He is running a research program at Aarhus University exploring the applicability of image fusion for guidance of regional anaesthesia - focusing on lumbosacral plexus blockade heading a team of PhD students. He has authored several papers and book chapters, is a busy reviewer, and has lectured about ultrasound guided regional anaesthesia topics around the world.
×
|
|





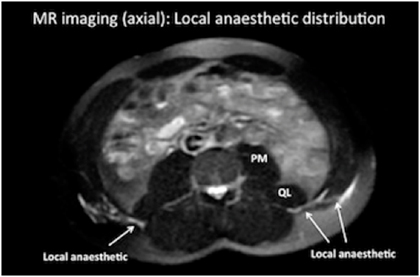
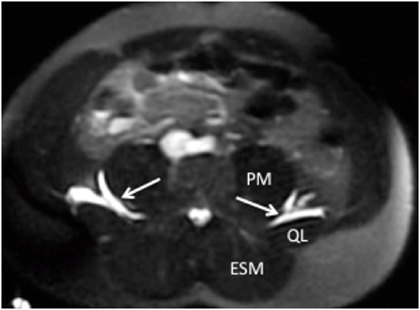
 A subsequent study by Børglum demonstrated redundant local anesthetic spread with the QLB1; i.e. lateral and a spread away from the site of injection (Figure 11).12
Figure 11. MRI scan showing dye and local anesthetic spread laterally and anteriorly after a QLB1 injection (Reference: Børglum et al)12
A subsequent study by Børglum demonstrated redundant local anesthetic spread with the QLB1; i.e. lateral and a spread away from the site of injection (Figure 11).12
Figure 11. MRI scan showing dye and local anesthetic spread laterally and anteriorly after a QLB1 injection (Reference: Børglum et al)12
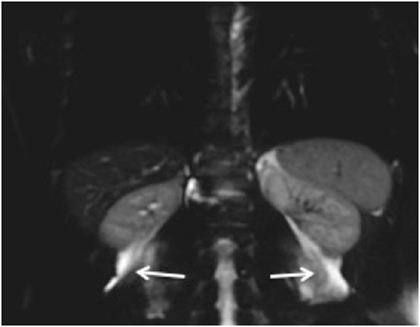
 Mechanism of Action (Anatomical Study)
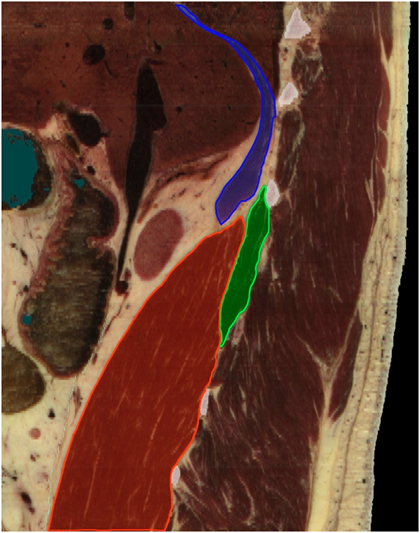
Below is a parasagittal view of the QL muscle, the psoas muscle and the diaphragm (Figure 14). Note that the cephalad parts of the QL muscle and the PM next to the diaphragm create a shape of a funnel which enables the injected local anesthetic trapped in the fascial plane between the two muscle to spread further into the thoracic paravertebral space below the diaphragm. This spread pattern is in accordance with the previous description by Saito.6
This is possible since the QL and PM muscles insert within the thoracic cage (i.e. 12th rib and vertebral body of T12 and disc, respectively) and since the transversalis fascia is continuous with the endothoracic fascia.
Figure 14. A parasagittal view of the quadratus lumborum muscle (green), the psoas muscle (PM) (red) and the diaphragm (blue).
Mechanism of Action (Anatomical Study)
Below is a parasagittal view of the QL muscle, the psoas muscle and the diaphragm (Figure 14). Note that the cephalad parts of the QL muscle and the PM next to the diaphragm create a shape of a funnel which enables the injected local anesthetic trapped in the fascial plane between the two muscle to spread further into the thoracic paravertebral space below the diaphragm. This spread pattern is in accordance with the previous description by Saito.6
This is possible since the QL and PM muscles insert within the thoracic cage (i.e. 12th rib and vertebral body of T12 and disc, respectively) and since the transversalis fascia is continuous with the endothoracic fascia.
Figure 14. A parasagittal view of the quadratus lumborum muscle (green), the psoas muscle (PM) (red) and the diaphragm (blue).