Anatomy
The transversalis fascia plane block, or TFP block, is a truncal block that targets the L1 nerve branches, namely the ilioinguinal and iliohypogastric nerves.The ilioinguinal and iliohypogastric nerves emerge from the lateral border of psoas major muscle, inferior to the 12th rib, and course over the anterior surface of the quadratus lumborum muscle. Lateral to the quadratus lumborum muscle, they initially run deep to transversus abdominis muscle for a variable distance before piercing the transversus abdominis muscle to enter the transversus abdominis plane between the internal oblique and transversus abdominis muscles.
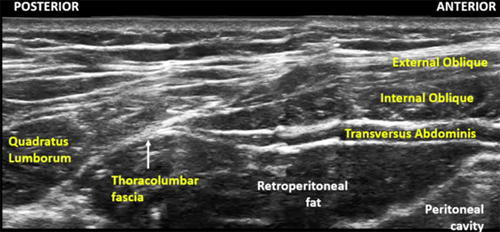
The TFP block targets the ilioinguinal and iliohypogastric nerves where they are between the fascia of the transversus abdominis muscle and the transversalis fascia. The fascia of the transversus abdominis muscle, also called the thoracolumbar fascia, is formed when the transversus abdominis and internal oblique muscles taper off posteriorly into a common aponeurosis and abuts the lateral border of quadratus lumborum muscle. The transversalis fascia is a thin aponeurotic membrane which lies between the transversus abdominis muscle and the extraperitoneal fascia, and is part of the general layer of fascia lining the abdominal cavity.
Anatomical Relationship of the Iliohypogastric and Ilioinguinal Nerves with the Surrounding Muscles

Anterior to the iliac crest, the nerves travel towards the anterior abdominal wall, piercing first the internal oblique muscle, and then the external oblique muscle. However the location at which this occurs varies widely between individuals.
The TFP block is indicated for pain relief following anterior iliac crest bone graft harvesting as the block is performed proximal to the L1 branches that innervate the anterior iliac crest. Local anesthetic spread can also involve the subcostal nerve (T12 spinal nerve). This block is also an analgesic option for inguinal hernia repair, open appendectomy and any surgery involving the L1 dermatome.
The TFP block is different from the transversus abdominis plane (TAP) block in a number of ways. The TFP block is designed to block the L1 nerve branches, which the TAP block does not reliably cover. The TFP block does not cover the dermatomes above L1 and T12 while the TAP block does. Local anesthetic is injected deep to the transversus abdominis muscle for the TFP block versus superficial to the muscle for the TAP block. The site of TFP injection is posterior to the mid-axillary line, unlike the classic ultrasound-guided TAP block.
Target Location of the Transversalis Fascia Plane Block