Scanning Technique

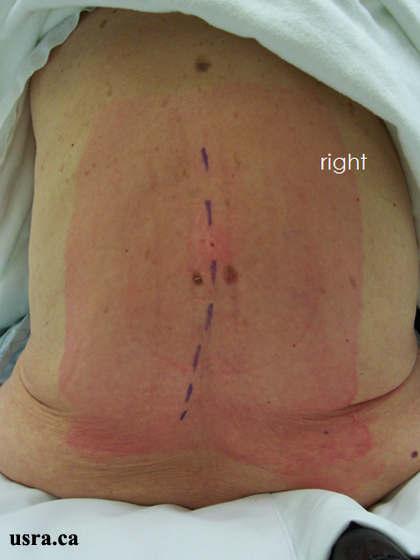
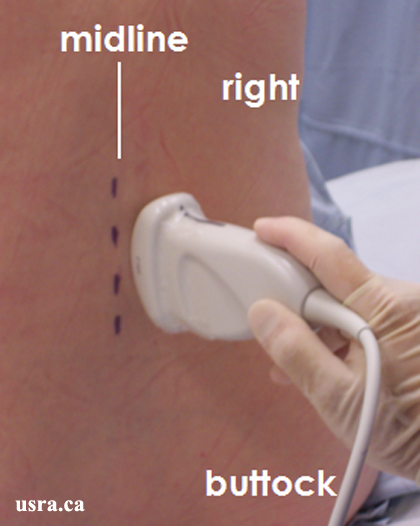
- Position the patient sitting, with the trunk flexed to widen the interspinous space.
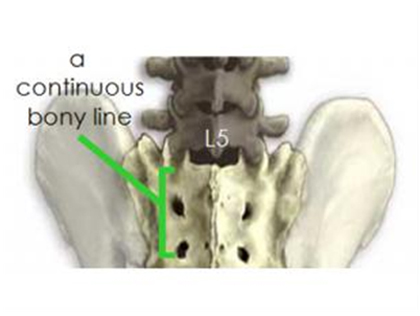
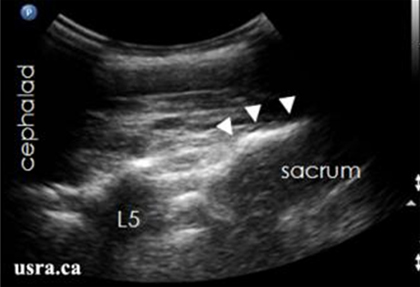
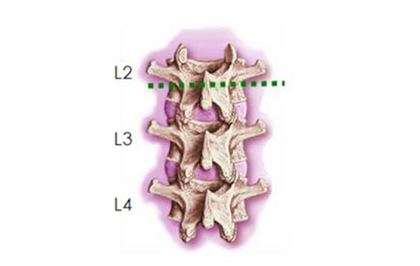
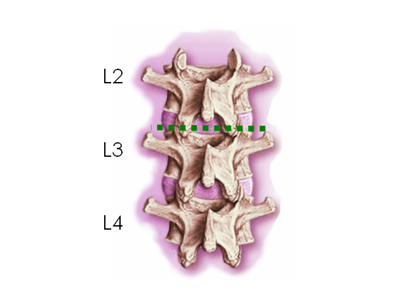
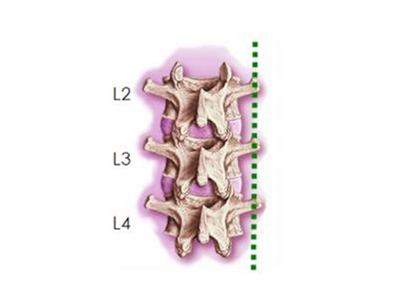
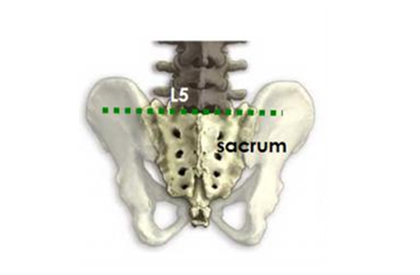
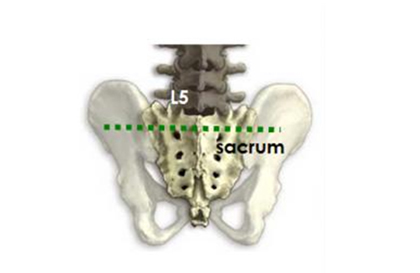
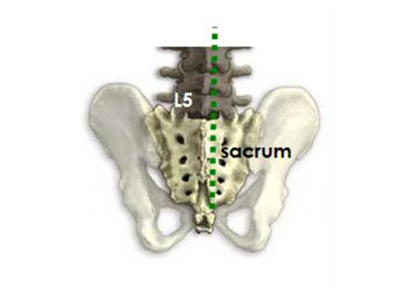
- Palpate the iliac crest on each side and mark the intercristal line (approximately at the L3-4 level).
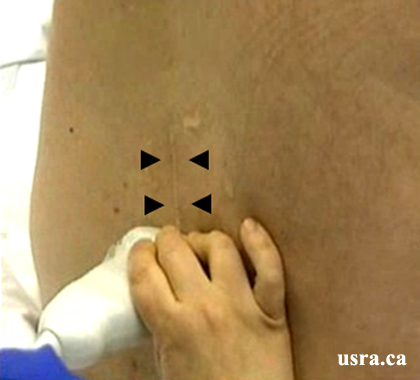
- Select a curved 2-5 MHz transducer and place the transducer in the transverse plane at the level of the L3 or L4 vertebra.
- Apply ample acoustic gel to ensure good transducer-to-skin contact and eliminate potential for air trapping (artifact).
- Adjust the appropriate depth of field (usually > 6-8 cm), focus range (usually > 5 cm) and gain.
Localization of the Epidural / Subarachnoid Space

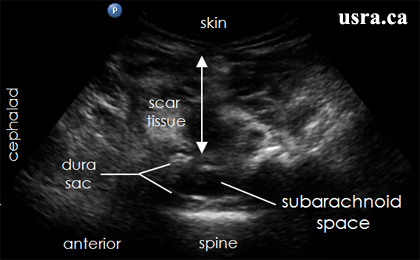
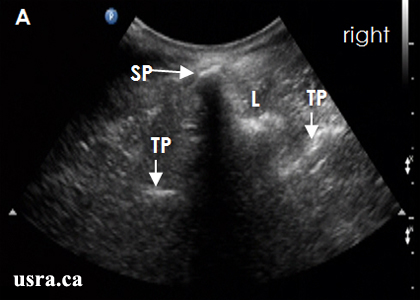
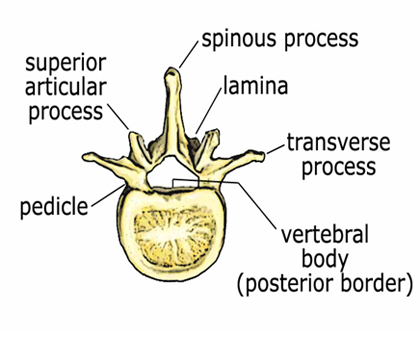
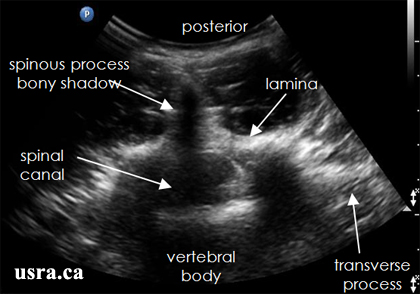
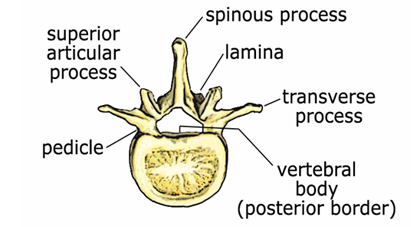
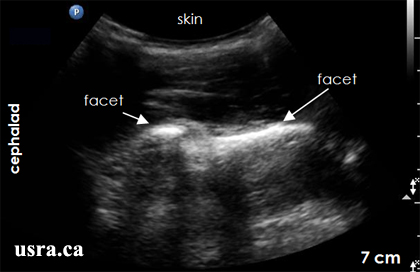
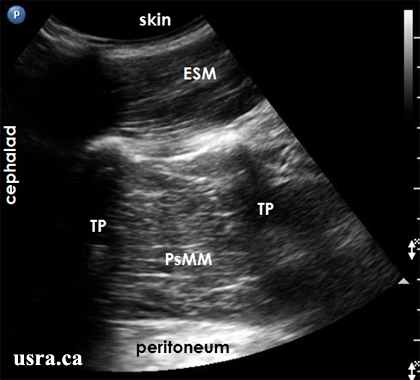
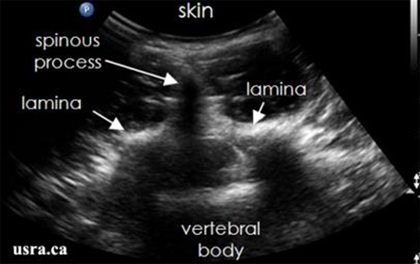
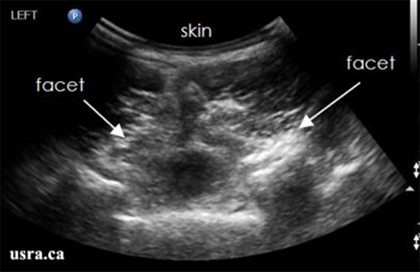
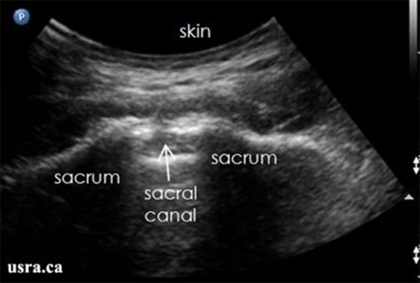
- The transverse ultrasound image reveals a superficial midline hypoechoic bony shadow that represents the posterior contour of the spinous process.
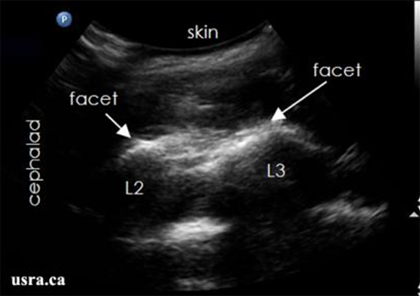
- Each lamina is visualized as a hyperechoic line anterolateral to the spinous process).
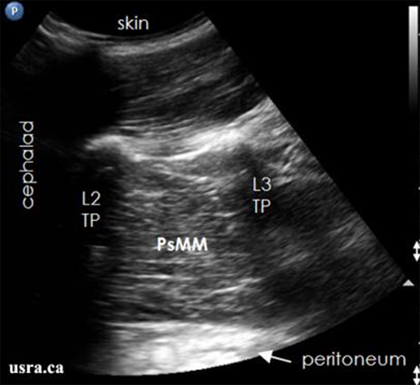
- Each transverse process is often visualized as a hyperechoic line located more lateral and anterior to the lamina.
Transverse Scan of the Spinous Process
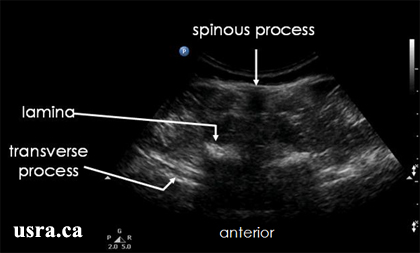

- The transverse ultrasound image reveals a superficial midline hypoechoic bony shadow that represents the posterior contour of the spinous
- Position the transducer so that the midpoint of the transducer is aligned with the midpoint of the spinous process.
- Mark the skin surface locations of the midline spinous process at several vertebral levels.
- Take note of the distance from the skin to:
- The spinous process
- The lamina
- The transverse process
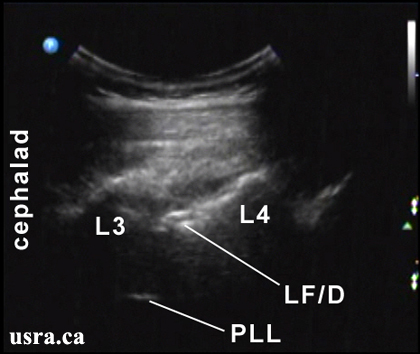
Next, visualize the interspinous space by moving the transducer cephalad
or caudad until the bony hypoechoic shadow of the spinous process
disappears.
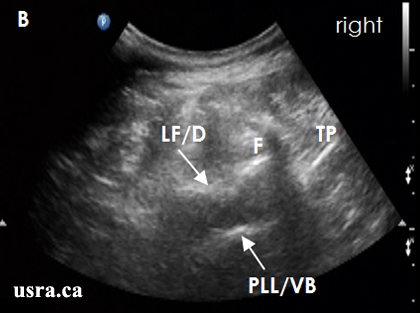
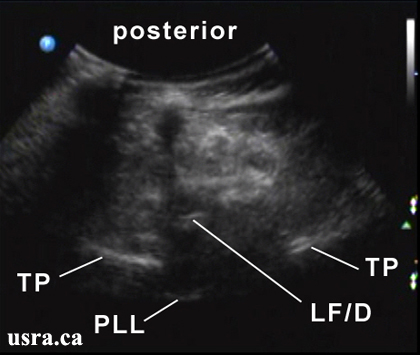
Transverse Scan of the Interspinous Space
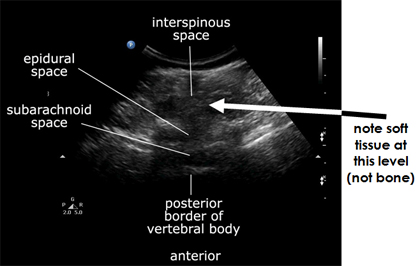

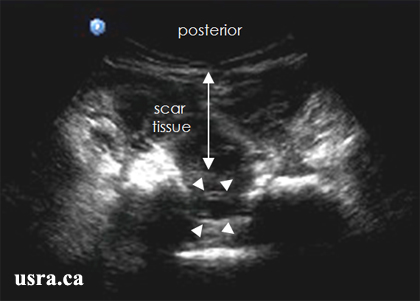
- Assess the size (width) of the interspinous space by slowly moving the transducer cephalad and caudad in the transverse plane. Alternatively, slightly angle the transducer cephalad and caudad to determine the size of the interspinous space.
- A narrow space is suggested when the bony shadows from two contiguous spinous processes are visualized with minimal transducer angulation.
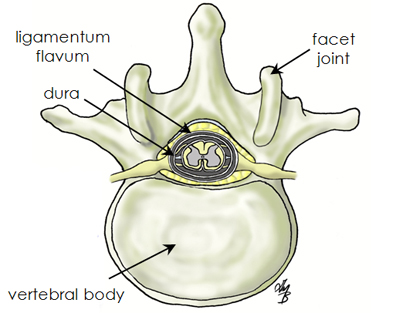
- Note the distance from the skin to the ligamentum flavum and the dura. It is not always possible to visualize the ligamentum flavum and the dura as two separate structures.
- It is common to see a single hyperechoic line representing the ligamentum flavum/dura complex.
- Finally, record the level of the interspinous space by placing a mark on each end of the transducer.

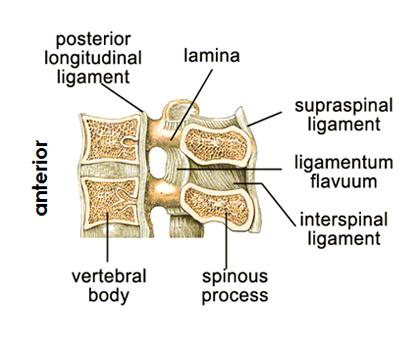
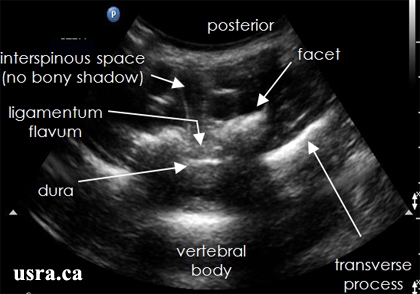
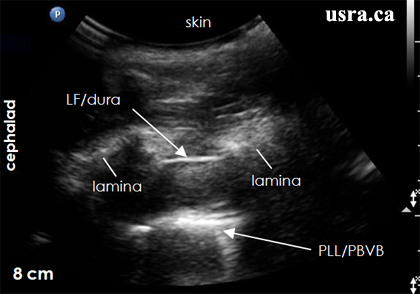
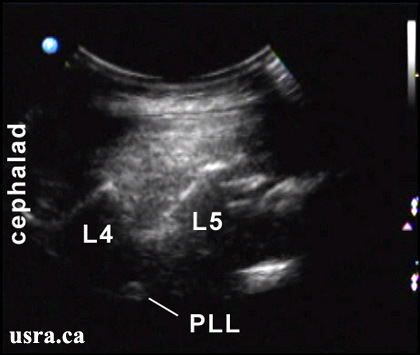
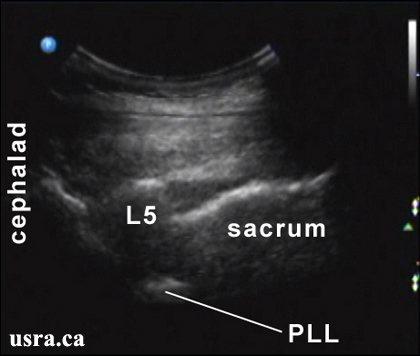
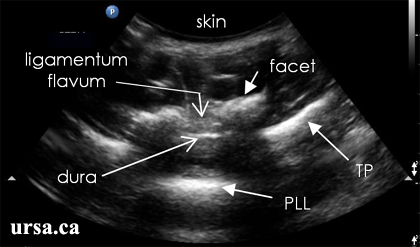 PLL = posterior longitudinal ligament
PLL = posterior longitudinal ligament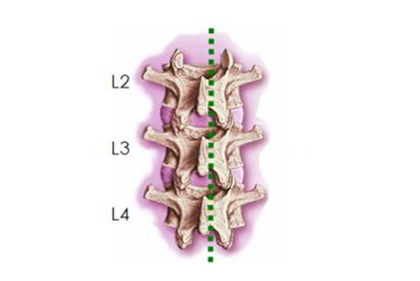
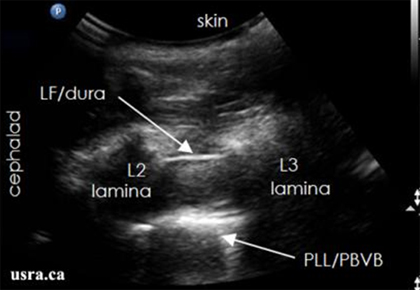 LF/dura = ligamentum flavum
LF/dura = ligamentum flavum 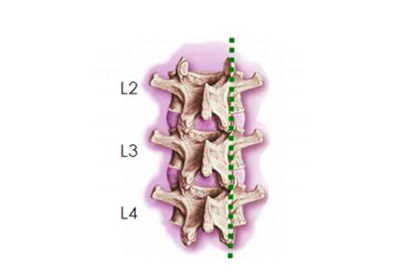
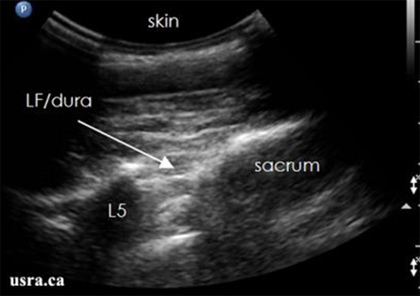 LF/dura = ligamentum flavum/dura complex
LF/dura = ligamentum flavum/dura complex