Needle Insertion Approach
- Ultrasound guided ankle block is considered a BASIC skill level block
because this is a superficial block.
- Both In Plane (IP) and Out of Plane (OOP) approaches can be used. The
IP approach is commonly used for single shot injection.
In Plane Approach
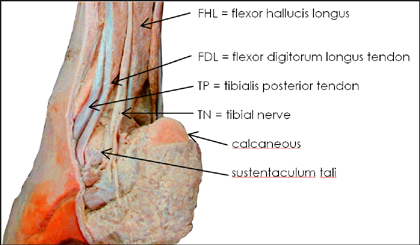
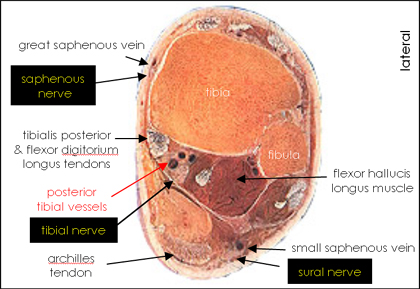
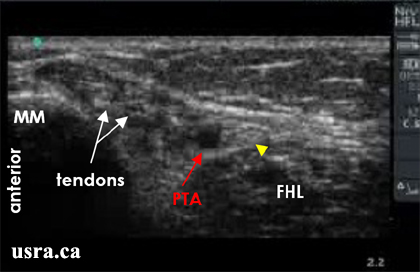
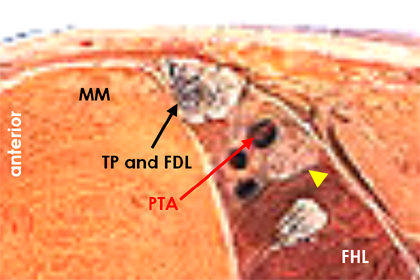
Tibial Nerve

|
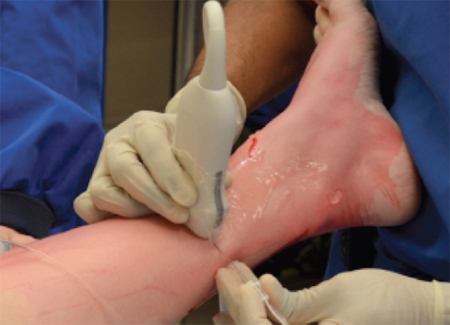
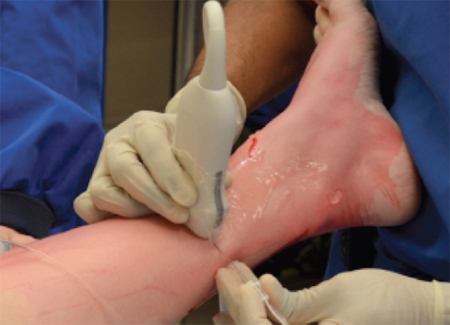
With the patient lying supine and the leg bolstered by a pillow,
insert a 4-5 cm 22-25 G needle inline with the ultrasound transducer
as seen in the picture.
|
- The needle is most conveniently inserted from the posterior end of the
transducer because the tibia bone located anteriorly obstructs needle
accessibility.
- To approach the nerve posteriorly from the side of the archilles tendon,
and to create some space between the bolster and the ankle for needle
access, it is best to have the leg rotated outward (laterally) or ask the
patient to turn slightly on the side.
- Aim to place the needle tip on each side of the tibial nerve without
puncturing the posterior tibial artery.
- Nerve stimulation is usually not necessary.
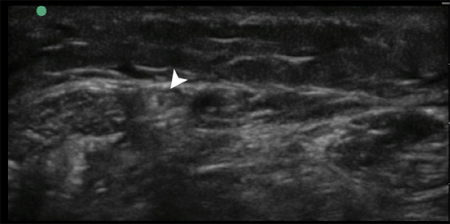
Superficial Peroneal Nerve

|
A 22 to 25 G needle can be inserted using an in plane approach and the
superficial peroneal nerve may be targeted above (usually easier) or
below the crural fascia.
|
Sural Nerve

|
A 22 to 25 G needle may be inserted using an in plane or out of plane approach.
|
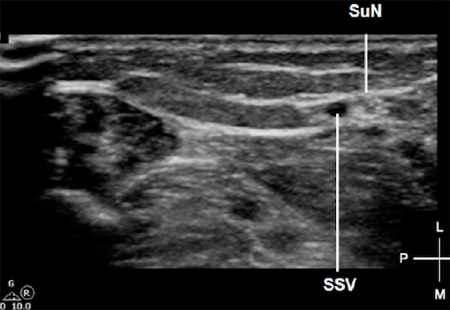
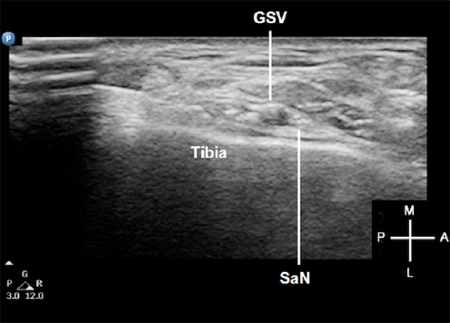
Saphenous Nerve
|
The saphenous nerve can be blocked using an in-plane or out-of-plane technique.
|
Out of Plane Approach
Tibial Nerve
- Patient positioning and needle insertion endpoint is similar to the in
plane approach.
- The advantage of the out of plane approach is needle accessibility to the
nerve and the ease of placing the needle tip on each side of the tibial
nerve. The tibia bone is no longer in the way of the needle path.
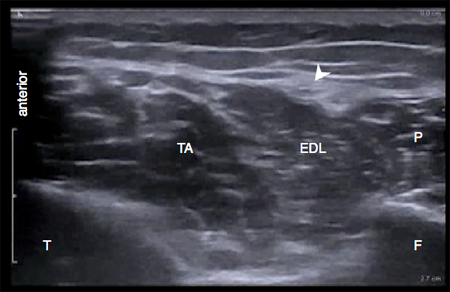
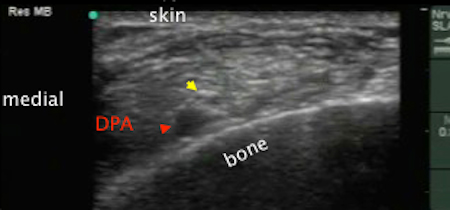
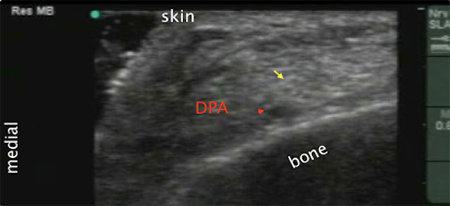
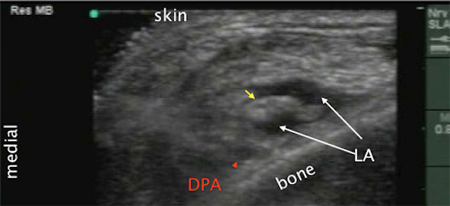
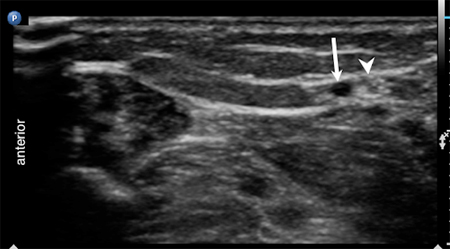
Deep Peroneal Nerve
- The deep peroneal nerve is a superficial branch that is located adjacent
to the dorsalis pedis artery at the ankle region.
- After skin and transducer preparation, place a 10-15 MHz transducer on the
dorsum of the foot along the intermalleolar line to locate the dorsalis
pedis artery in the transverse (short axis) view.
- Aim to find the predominantly hypoechoic deep peroneal nerve lateral to the
dorsalis pedis artery and the extensor hallucis longus tendon. This nerve
is small thus visualization can be difficult.

|
A 25 G 2.5 mm needle can be inserted using the out of plane approach.
|


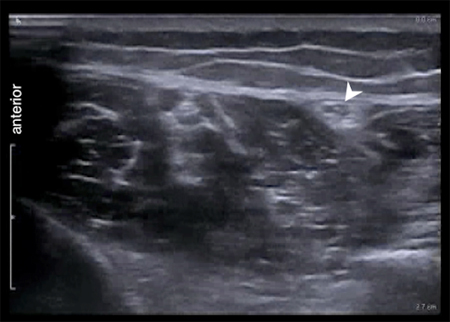
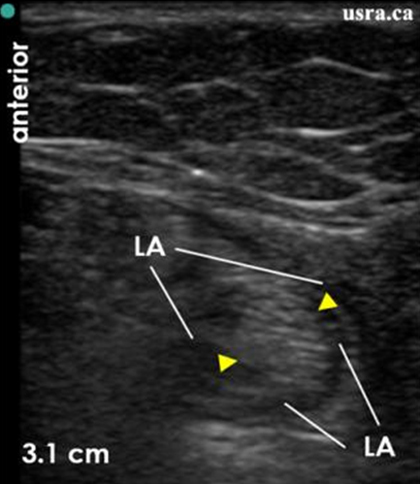
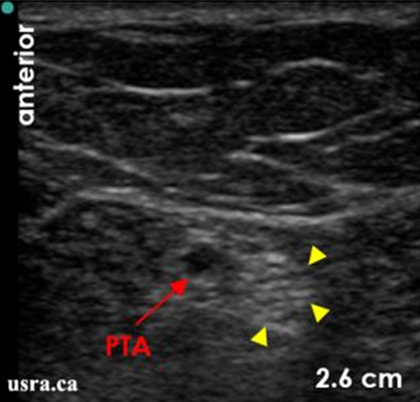 Transverse View
Transverse View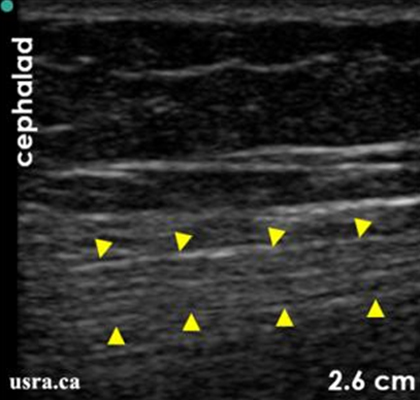 Longitudinal View
Longitudinal View

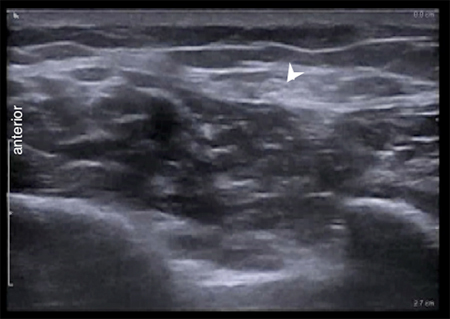







 Transverse View
Transverse View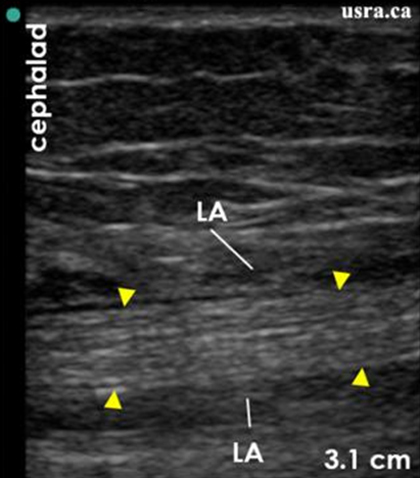 Longitudinal View
Longitudinal View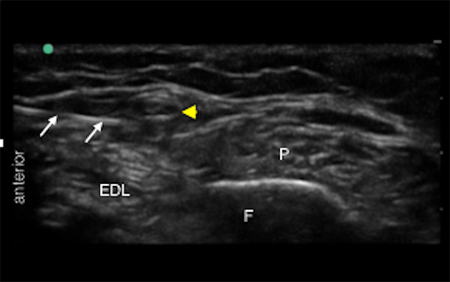
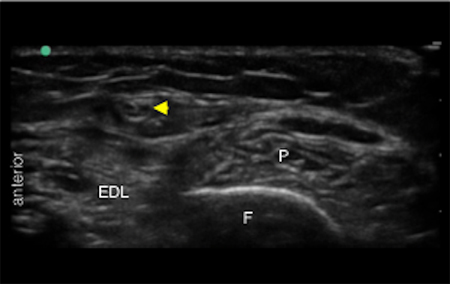
 Pre Injection
Pre Injection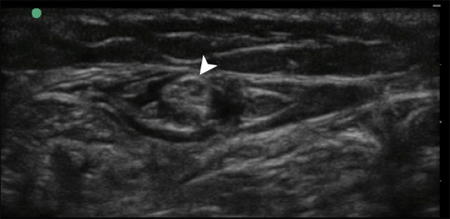 Post Injection
Post Injection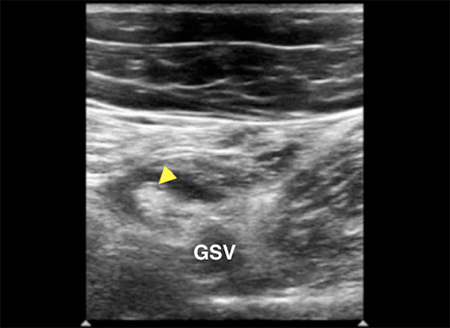

 Pre Injection
Pre Injection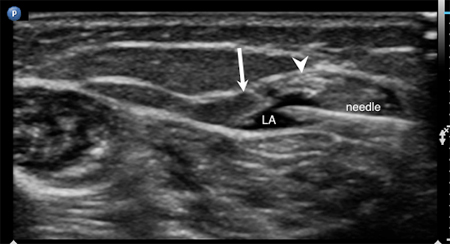 Post Injection
Post Injection