Image Gallery
1. Local Anesthetic Spread Around the Sciatic Nerve
|
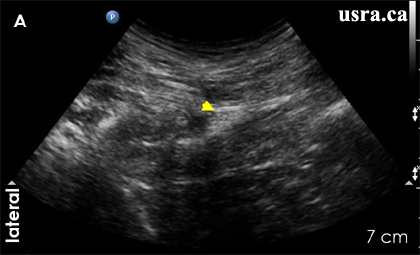
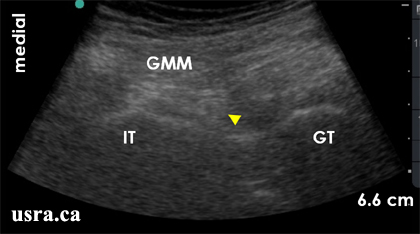
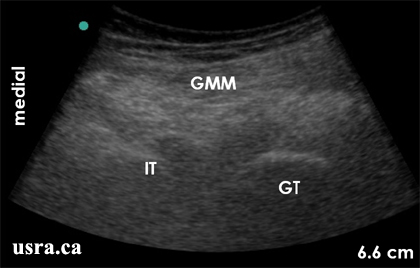
A. Pre Injection
The sciatic nerve is predominantly hyperechoic and elliptical in this transverse view.
Arrowhead = sciatic nerve
|
|
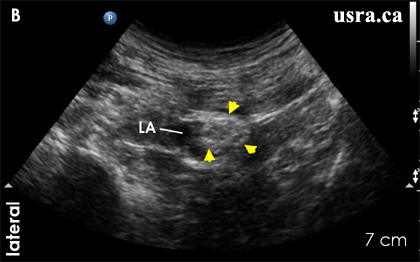
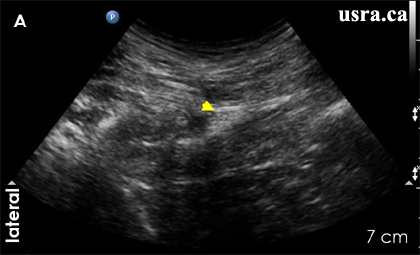
B. Post Injection
The sciatic nerve is now surrounded by a hypoechoic collection of local anesthetic (LA).
The nerve is now round in shape. Local anesthetic spread is not circum-ferential.
Arrowhead = sciatic nerve
|
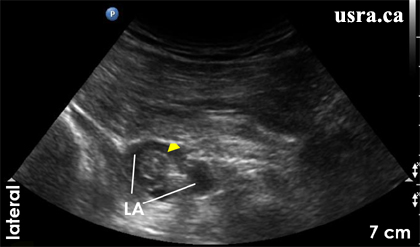
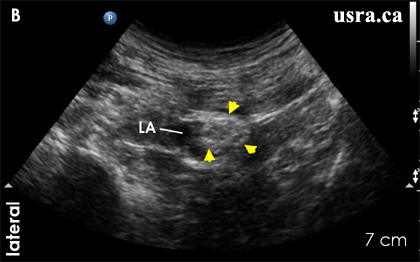
2. Apparent Nerve Enlargement After Local Anesthetic Injection
|
The nerve diameter is noted to be wider after injection suggesting some degree
of unintentional intraneural injection.
Arrowhead = sciatic nerve
LA = local anesthetic
|
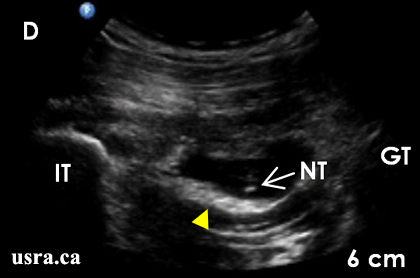
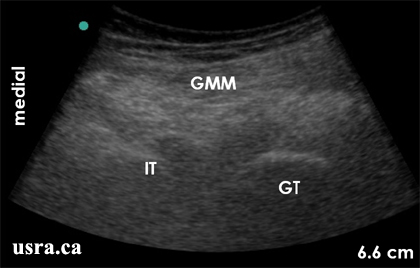
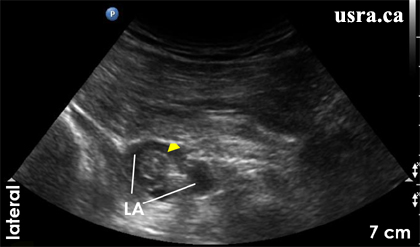
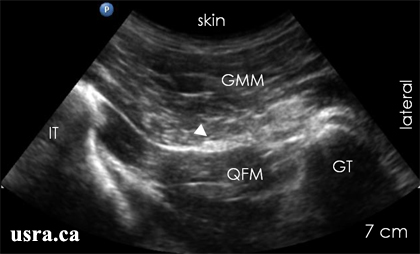
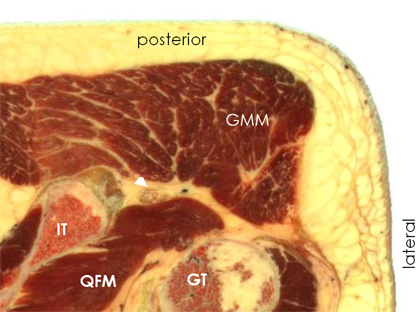
3. Poor Nerve Visualization
|
Pre Injection
The subgluteal sciatic nerve may not be clearly visualized (up to 30% in
the author’s opinion). However, it is always possible to identify the
muscular and bony landmarks.
GMM = gluteus maximus muscle
GT = greater trochanter
IT = ischial tuberosity
|
|
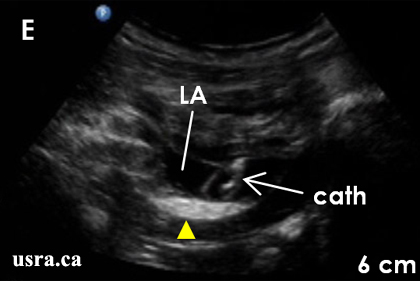
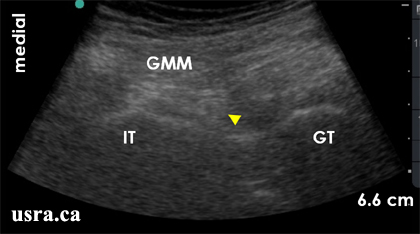
Post Injection
The sciatic nerve (arrowhead) is now visualized after local anesthetic
injection.
GMM = gluteus maximus muscle
GT = greater trochanter
IT = ischial tuberosity
|
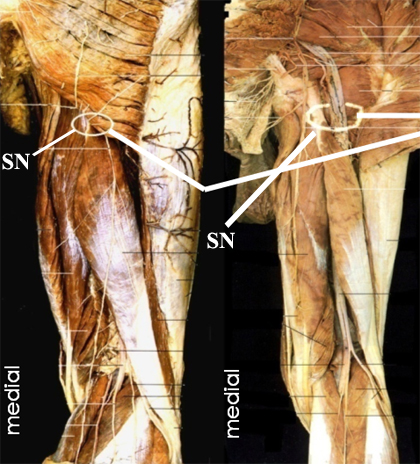
Notes: When nerve visualization is difficult, it is extremely helpful to
combine nerve stimulation with ultrasound for nerve localization. The sciatic
nerve is expected to lie deep to the gluteus maximus muscle (GMM) and between
the greater trochanter (GT) and ischial tuberosity (IT).
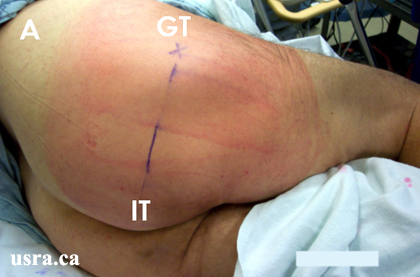
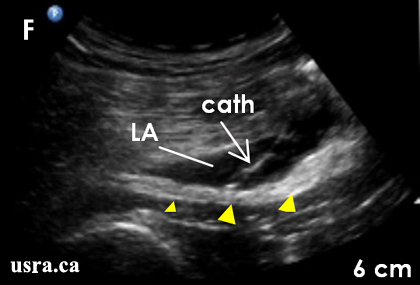
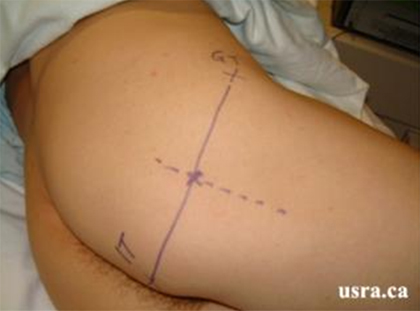
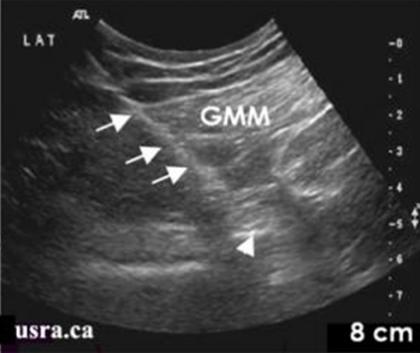
4. A Thick Adipose Layer

|
Arrows = thickness of the adipose tissue
Arrowhead = sciatic nerve
|



 Arrowhead = sciatic nerve
Arrowhead = sciatic nerve 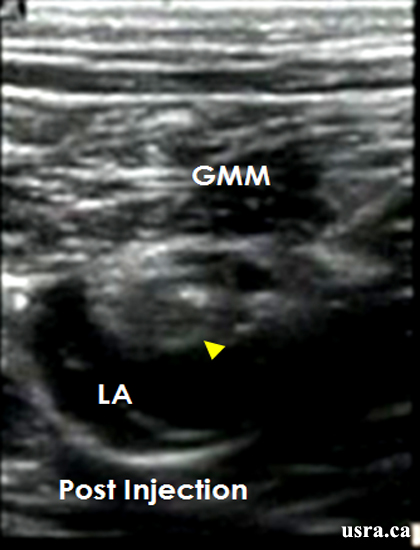 Arrowhead = sciatic nerve
Arrowhead = sciatic nerve