Scanning Technique
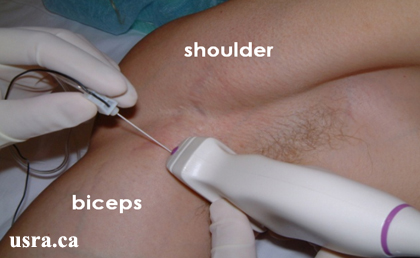
- Position the patient supine and abduct the arm to 90 degrees.
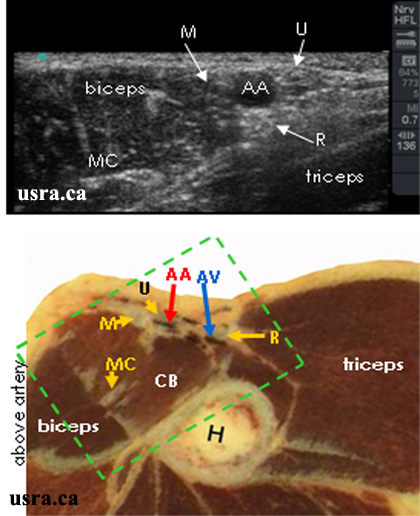
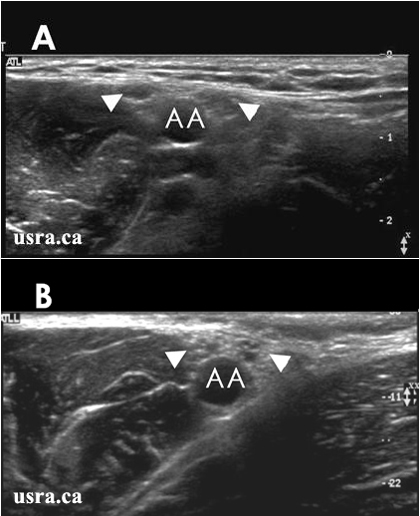
- After skin and transducer preparation (see transducer preparation section), place a linear 38-mm, high frequency 10-12 MHz transducer firmly in the transverse plane along the axillary crease to obtain the best possible transverse view of the brachial plexus.
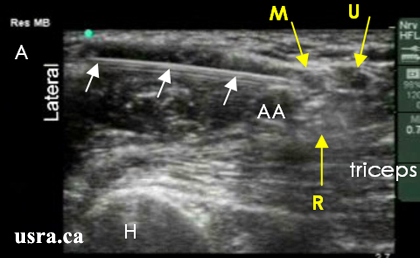
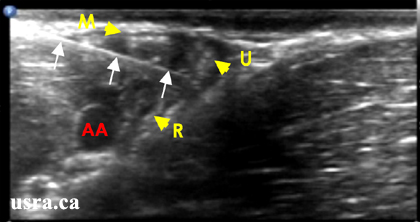
- Optimize machine imaging capability. Select appropriate depth of field (within 1-2 cm), focus range (usually within 1 cm) and gain.
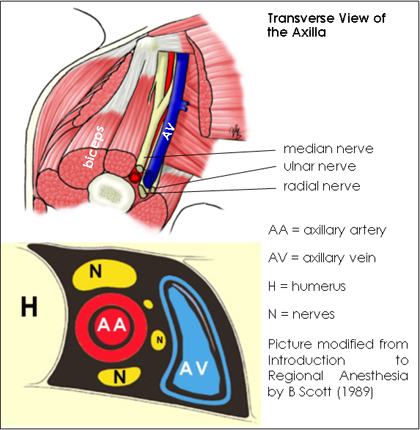
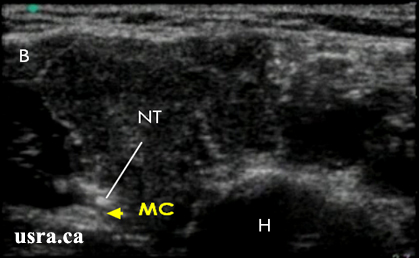
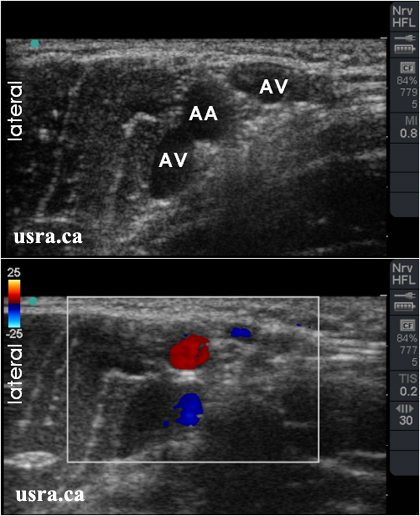
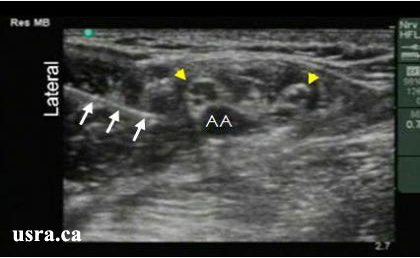
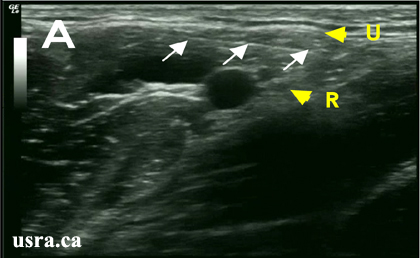
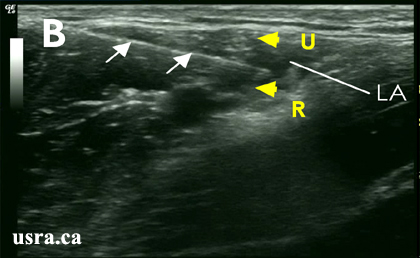
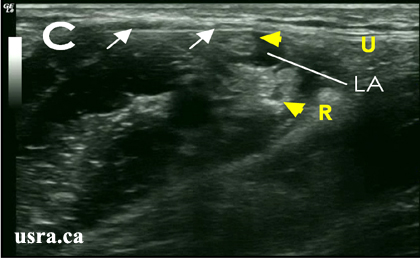
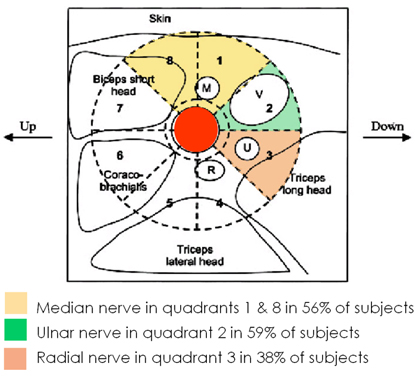
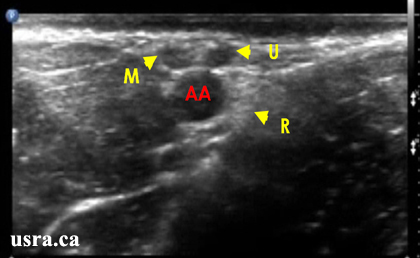
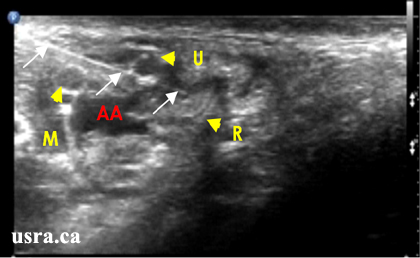
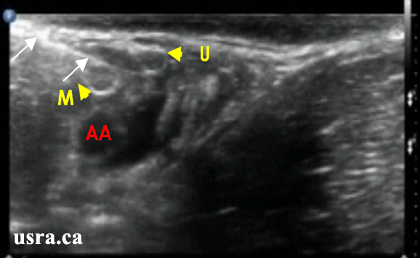
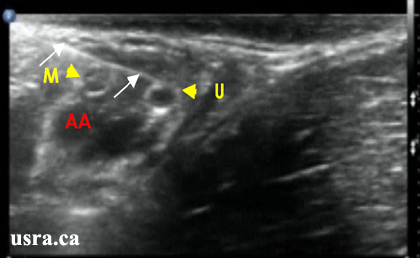
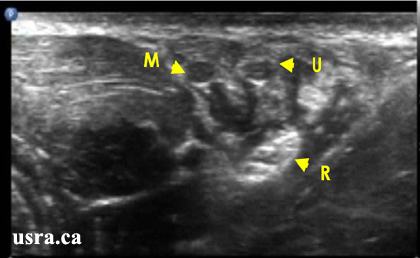
- Visualize the median, ulnar, radial and musculocutaneous nerves in the transverse view(short axis). Nerves in the axilla have mixed echogenicity and a honey comb appearance (representing a mixture of hypoechoic nerve fasiscles and hyperechoic connective tissues). The nerves are round or oval, and are located next to the axillary artery and vein(s).