Anatomy
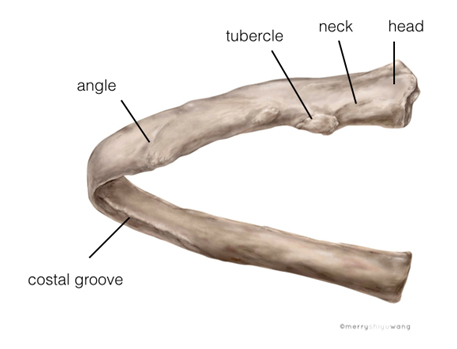
The intercostal space (ICS) is the space between 2 adjacent ribs of the thoracic cage. A typical rib (rib 3rd to 10th) has the following structures: head, neck, tubercle, angle and body Figure 1). Typically a rib courses oblique as it curves laterally and anteriorly and so is the intercostal space. Note that the costal groove in the inferior border of the rib ends as it courses more anteriorly (Figure 1).
Figure 1. Anatomy of a rib
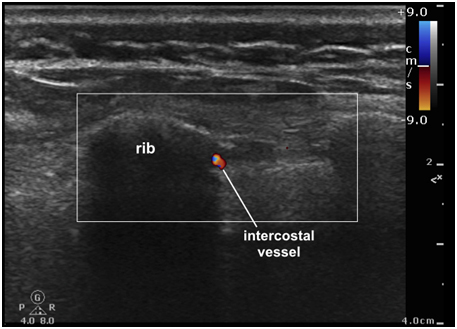
There are 11 ICSs on each side and the content of each ICS includes: intercostal muscles, intercostal membranes, intercostal nerves (ICNs) and intercostal vessels (Figure 2). Deep to the intercostal space is the parietal pleura. Lateral to the costal angle, the ribs and ICSs are superficial thus easily palpable on the back.
Figure 2. Posterior view of the intercostal nerves running through the posterior intercostal spaces between two ribs. The erector spinae muscle is completely removed and the external intercostal muscles are partially removed in this dissection
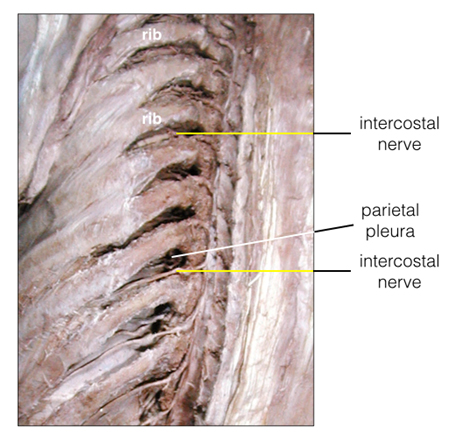
There are 11 pairs of ICNs (T1-T11) which are anterior divisions of the thoracic spinal nerves. They course through the intercostal spaces accompanied by the intercostal vessels. They provide sensory and motor innervation to the thoracic and abdominal wall and sensory innervation to the parietal pleura and peritoneum.
At the posterior axillary line, the ICNs divide in main and collateral branches. The former is found near the inferior border of the upper rib of an ICS and the latter follows the superior border of the lower rib (note that the intercostal vessels also branch in the same pattern.
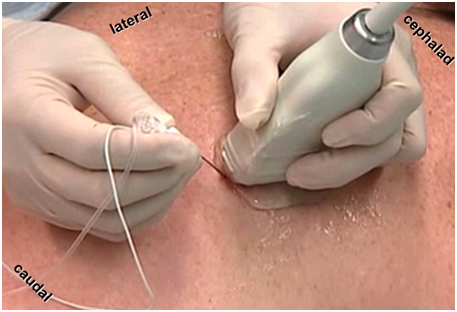
Moreover, approximately at the midaxillary line, the ICNs give off the lateral cutaneous branches which further divide into anterior and posterior cutaneous terminal branches. To ensure complete sensory blockade, it is therefore important to anesthetize the intercostal nerves at or posterior to the posterior axillary line.
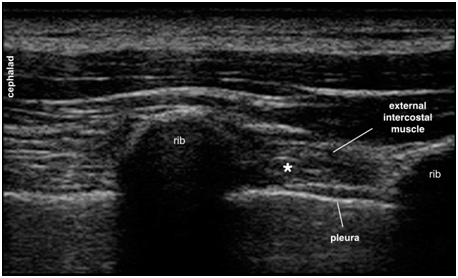
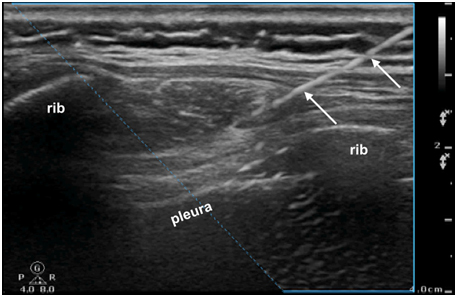
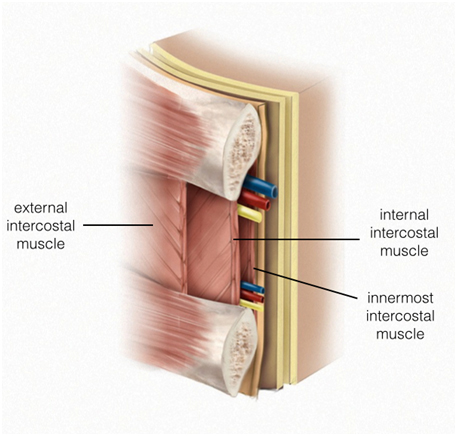
Lateral to the costal angle, there are 3 layers of muscles? external intercostal muscle (EICM), the internal intercostal muscle (IICM) and the innermost intercostal muscle (IMICM) (Figure 3). The innermost intercostal muscle, also called the intercostalis intimus muscle, is a flimsy innermost muscle layer which readily permits local anesthetic diffusion. Deep to the innermost intercostal muscle is the parietal pleura. From the costal angle onwards, the main ICNs and vessels, grouped as a neurovascular bundle, are arranged in the vein, artery and nerve (VAN) orientation from superior to inferior. Note that this constant arrangement does not apply for the collateral bundle. Both neurovascular bundles are found between the internal intercostal muscle and innermost intercostal muscle but the main bundle is found within the costal groove or near the inferior margin of the upper rib of an ICS while the collateral bundle is found at the superior border of the lower rib.
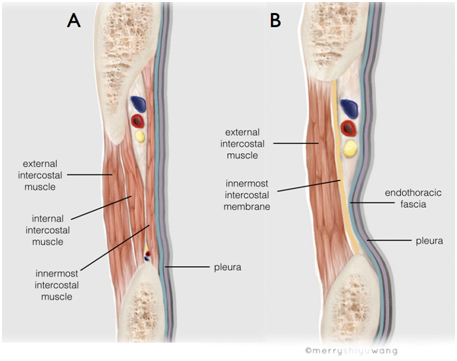
Figure 3. Schematic diagram of the content of the anterior ICS (anterior to the posterior axillary line) after the IC neurovascular bundle has divided into the main and collateral branches
Medial to the costal angle, there is only 1 layer of muscle, the external intercostal muscle and an internal intercostal membrane (IICMe, Figure 4). There is no internal intercostal muscle. The intercostal neurovascular bundle runs between the ribs, deep to the internal intercostal membrane and superficial to the endothoracic fascia (ETF). There is no clear intercostal groove in this location. Deep to the endothoracic fascia is the parietal pleura.
Figure 4. Content of the posterior ICS (posterior to posterior axillary line) lateral to the costal angle (A) and medial to the costal angle (B). It shows the location of the intercostal nerve and vessels in relationship to the intercostal musculature and pleura