Phantom Practice STEPS TO BUILD A PORCINE PHANTOM
- Prepare a piece of pork shoulder with the humerus attached.
- Carve to 20 cm x 12 cm x 8 cm (length x width x height).
- Remove the skin and deodorize the pork specimen by soaking it in approximately 30 mL of 70% alcohol inside a plastic bag for 8 to 10 hours at 4°C.
- Use a metal or plastic rod (approximately 1.5 cm in diameter) to create a 10cm long tunnel within the muscle layers approximately 3 cm from the surface.
- Insert a bovine tendon (approximately 8 cm long and 1 cm in diameter) inside the tunnel; ultrasound appearance of tendon and nerve is similar.
- Use a smaller tendon for advanced practice.
- Wrap up the whole phantom in a transparent para film and reinforce exteriorly by a surgical paper towel.
- Store specimen at 4°C until use.
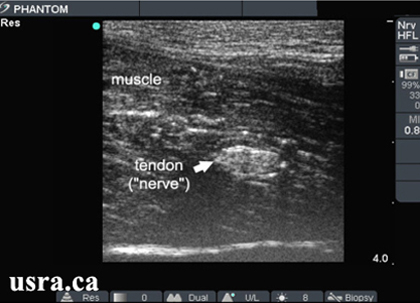
Short axis (x-section) view |

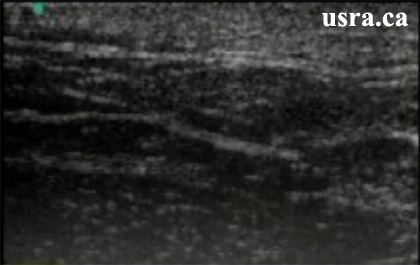
Longitudinal view |
In Plane Needle Insertion Practice
A. The needle is inserted in plane with the transducer but the needle image is not seen.

|
|
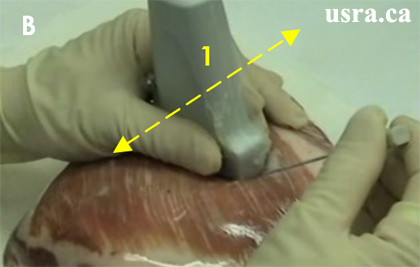
B. Maneuver # 1: Slide the transducer back and forth slowly over the needle until the needle image is seen. Hold the needle steady.
|

|
C. Maneuver # 2: Wiggle the needle tip from side to side until the needle is seen. Hold the transducer steady.

|
|
Out of Plane Needle Insertion Practice
Please refer to Needle Localization.

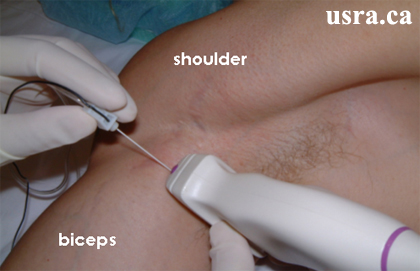

 This is an example of a right handed operator using the right hand to hold the needle for a left sided interscalene block. Note that the operator is standing on the left side of the patient below the clavicle.
This is an example of a right handed operator using the right hand to hold the needle for a left sided interscalene block. Note that the operator is standing on the left side of the patient below the clavicle.
 This is an example of a right handed operator using the right hand to hold the needle for a right sided interscalene block. Note that the operator is now standing on the right side of the patient above the clavicle.
This is an example of a right handed operator using the right hand to hold the needle for a right sided interscalene block. Note that the operator is now standing on the right side of the patient above the clavicle.
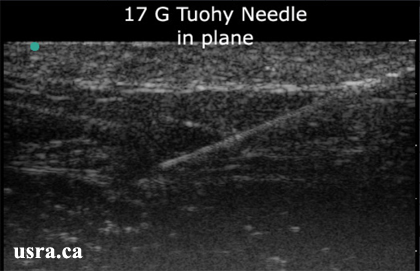 A 17 G Tuohy needle inserted in plane with the ultrasound transducer at an approximately 45 degree angle
A 17 G Tuohy needle inserted in plane with the ultrasound transducer at an approximately 45 degree angle
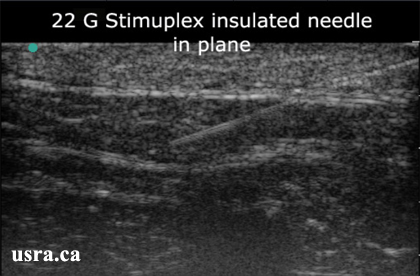 A 22 G insulated needle inserted in plane with the transducer at an approximately 45 degree angle
A 22 G insulated needle inserted in plane with the transducer at an approximately 45 degree angle

 An example of the echogenic tip needle by HakkoTM Medical Co. LTD (Japan).
An example of the echogenic tip needle by HakkoTM Medical Co. LTD (Japan). Proper operator and screen orientation; note that the ultrasound machine is placed directly in front of the operator to provide a direct line of vision.
Proper operator and screen orientation; note that the ultrasound machine is placed directly in front of the operator to provide a direct line of vision.
 Improper operator and screen orientation; note that the operatorís head is turned almost 90 degrees to view the ultrasound image on the screen.
Improper operator and screen orientation; note that the operatorís head is turned almost 90 degrees to view the ultrasound image on the screen.
 Proper body position and bed height for the procedure
Proper body position and bed height for the procedure
 Improper body position; the bed is too low for the procedure
Improper body position; the bed is too low for the procedure
 Proper transducer holding skill; the hand is placed close to the transducer contact surface
Proper transducer holding skill; the hand is placed close to the transducer contact surface
 Improper transducer holding position; the hand is high up on the transducer
Improper transducer holding position; the hand is high up on the transducer
 Proper hand and arm positions; both hands and arms are comfortably supported
Proper hand and arm positions; both hands and arms are comfortably supported
 Improper hand and arm positions; both the arm holding the transducer and the hand holding the needle are not supported
Improper hand and arm positions; both the arm holding the transducer and the hand holding the needle are not supported
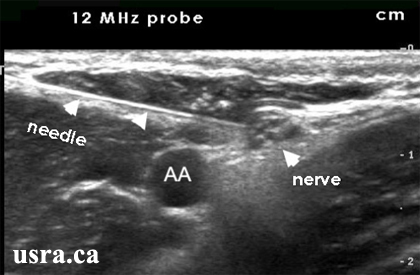
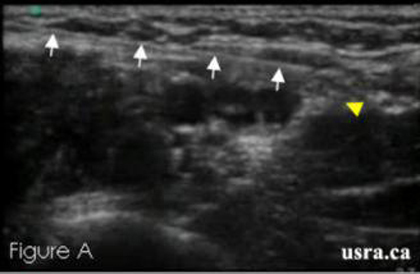 Figure A shows needle in contact with nerve
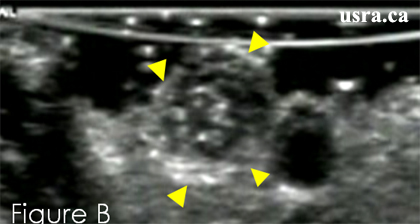
Figure A shows needle in contact with nerve 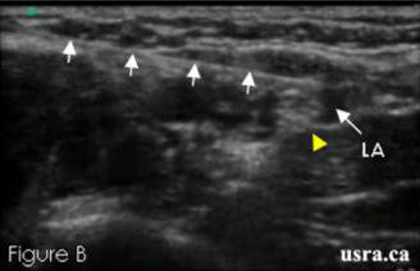 Figure B show local anesthetic injection around the nerve
Figure B show local anesthetic injection around the nerve 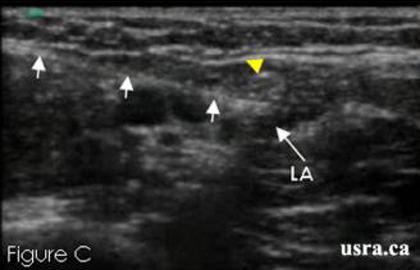 Figure C show local anesthetic injection around the nerve
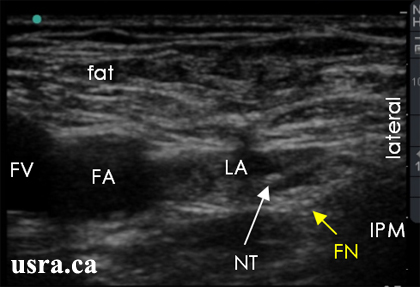
Figure C show local anesthetic injection around the nerve  Figure A shows an improper injection outside the fascia iliaca (FI). Arrows show tissue expansion outside the fascia.
Figure A shows an improper injection outside the fascia iliaca (FI). Arrows show tissue expansion outside the fascia.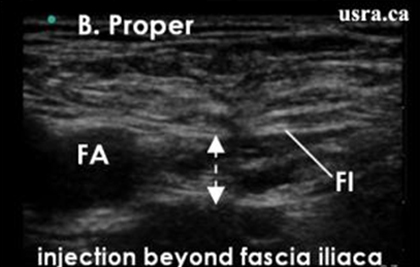 Figure B shows a proper injection deep to the fascia iliaca (FI). Arrows show fluid expansion deep to the fascia.
Figure B shows a proper injection deep to the fascia iliaca (FI). Arrows show fluid expansion deep to the fascia.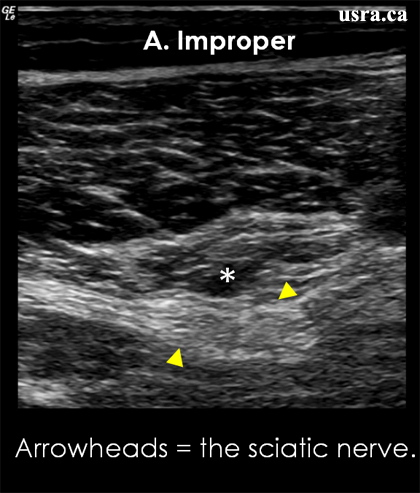 Figure A illustrates improper injection and subsequent hypoechoic local anesthetic spread (asterisk) outside the fascial sheath of the sciatic nerve (hyperechoic structure) in the popliteal region.
Figure A illustrates improper injection and subsequent hypoechoic local anesthetic spread (asterisk) outside the fascial sheath of the sciatic nerve (hyperechoic structure) in the popliteal region.
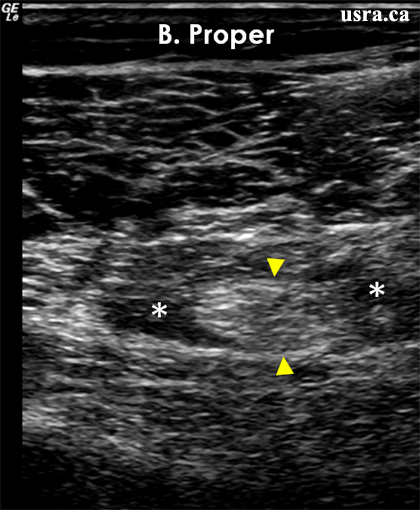 Figure B illustrates proper injection (asterisks) inside the fascia sheath of the sciatic nerve.
Figure B illustrates proper injection (asterisks) inside the fascia sheath of the sciatic nerve.
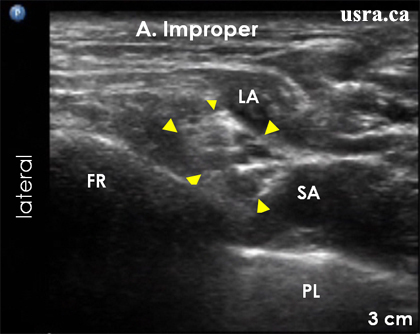 Figure A illustrates improper injection and hypoechoic local anesthetic (LA) spread outside the brachial plexus sheath.
Figure A illustrates improper injection and hypoechoic local anesthetic (LA) spread outside the brachial plexus sheath.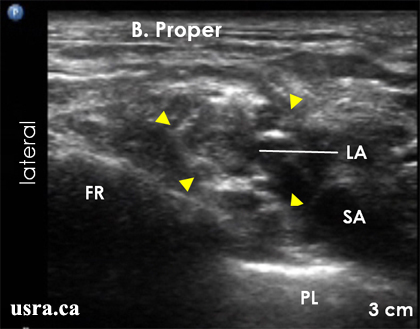 Figure B illustrates proper injection (LA) inside the expanded brachial plexus sheath.
Figure B illustrates proper injection (LA) inside the expanded brachial plexus sheath.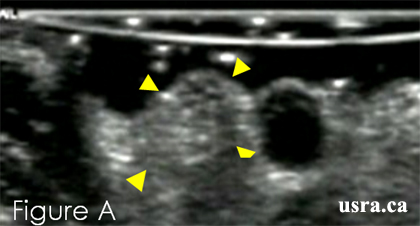 Pre-injection
Pre-injection
 Post-injection
Post-injection
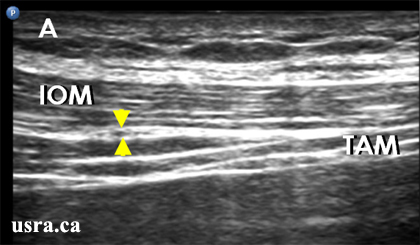 Figure A shows hypoechoic ilioinguinal/iliohypogastric nerves (arrowheads) within the plane between the internal oblique muscle (IOM) and the transverse abdominis muscle (TAM).
Figure A shows hypoechoic ilioinguinal/iliohypogastric nerves (arrowheads) within the plane between the internal oblique muscle (IOM) and the transverse abdominis muscle (TAM).
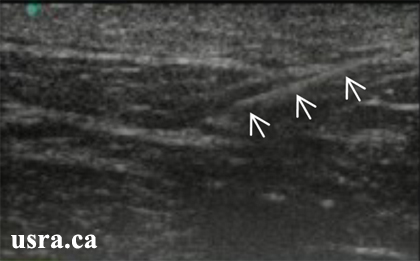
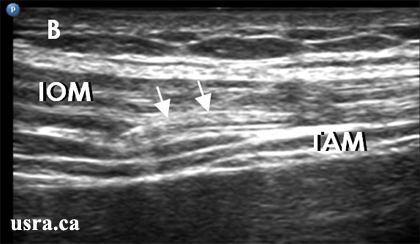 Figure B shows needle (arrows) approaching the nerves using the in plane needle approach. It is difficult to tell if the needle tip is indeed inside the intermuscular plane.
Figure B shows needle (arrows) approaching the nerves using the in plane needle approach. It is difficult to tell if the needle tip is indeed inside the intermuscular plane.
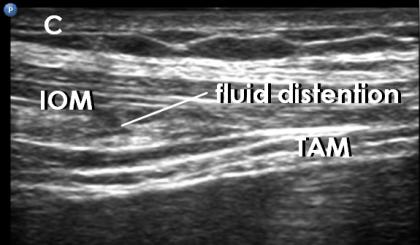 Figure C shows injection of a small amount of fluid ("hydro dissection") to open up the narrow plane. A small hypoechoic fluid collection is now seen above the nerves.
Figure C shows injection of a small amount of fluid ("hydro dissection") to open up the narrow plane. A small hypoechoic fluid collection is now seen above the nerves.