Anatomy
The cervical sympathetic trunk, one on each side of the vertebral bodies, carries sympathetic fibers to the head and neck structures. The cervical sympathetic trunk has 3 ganglia: superior, middle and inferior ganglia (Figure 1).
Figure 1. Coronal section of the neck showing the cervical sympathetic trunk and its relation to the prevertebral muscles on each side
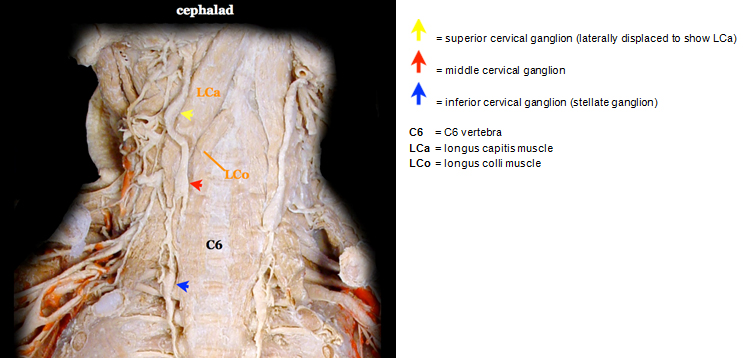
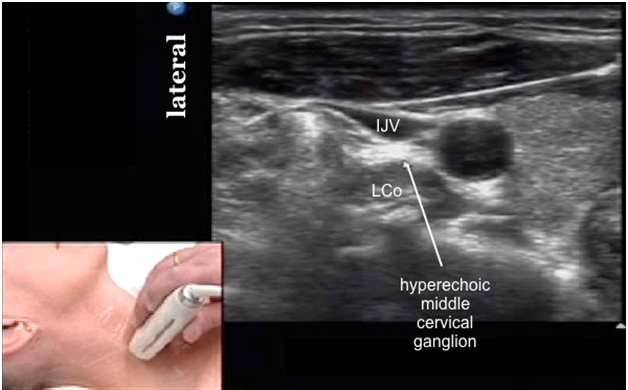
The superior cervical ganglion containing C1-4 fibers is usually found opposite the C2 and C3 vertebrae. The middle cervical ganglion containing C5 and C6 fibers is often found opposite the C6 vertebrae. It is the smallest of the 3 cervical ganglia and may be absent. The inferior cervical ganglion containing C7 and C8 fibers is often located between the base of the C7 transverse process and the neck of the 1st rib, on the medial side of the costocervical artery.
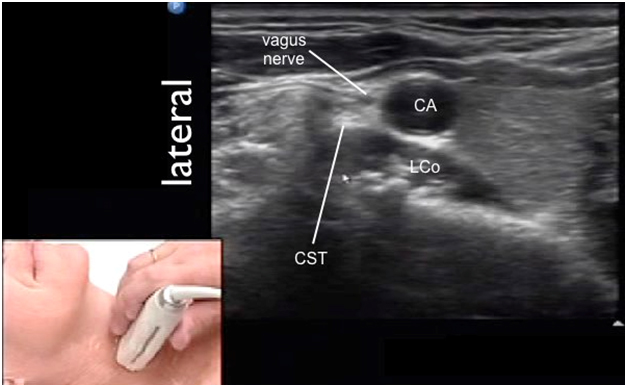
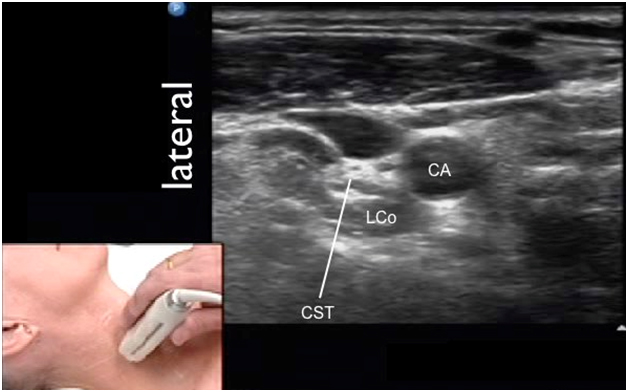
Movie 1. Cervical sympathetic ganglia and trunk anatomy
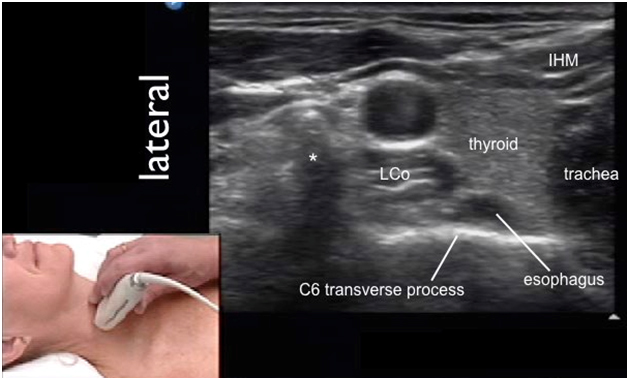
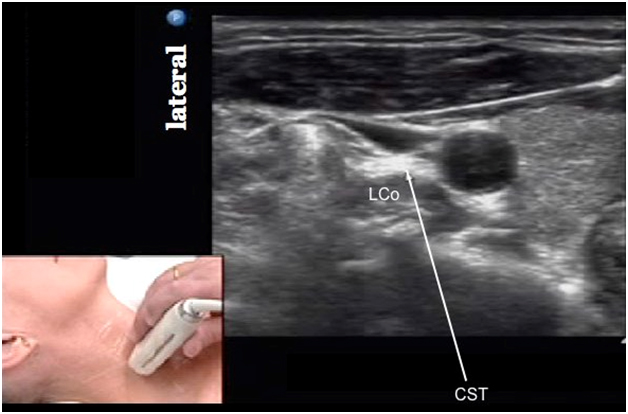
When the inferior cervical ganglion is fused with the T1 ganglion, this cervicothoracic ganglion is called the stellate ganglion. It is often situated posterior to the vertebral artery and the subclavian artery and lateral to the trachea, esophagus and the longus colli muscle. The post-ganglionic fibers of the stellate ganglion provide sympathetic innervation to the upper limbs.
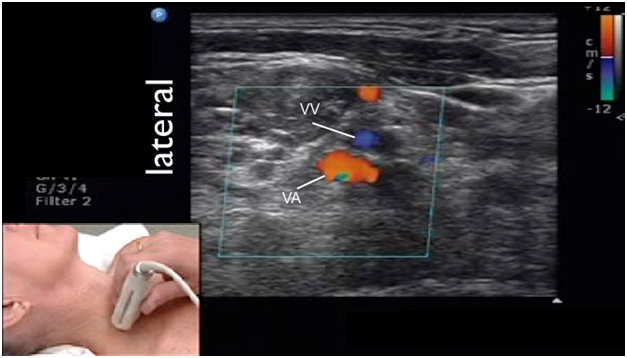
Movie 2. Stellate ganglion anatomy
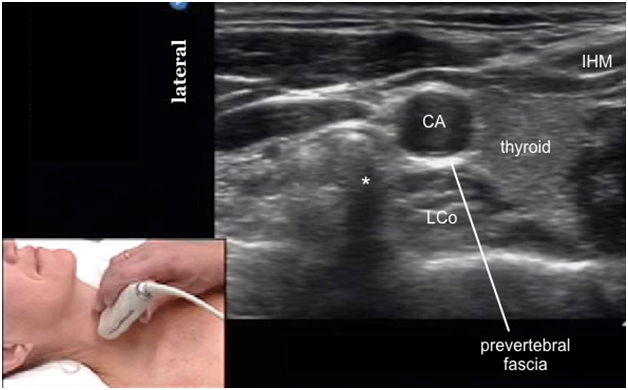
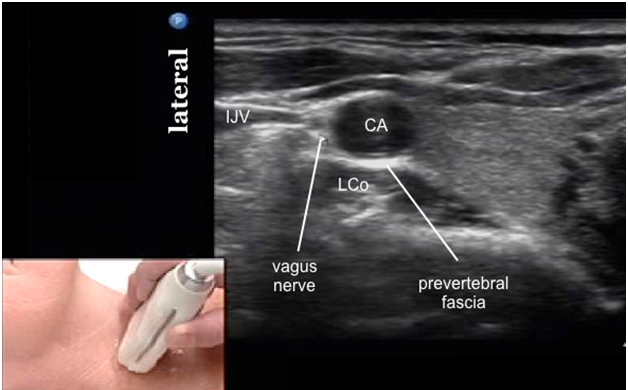
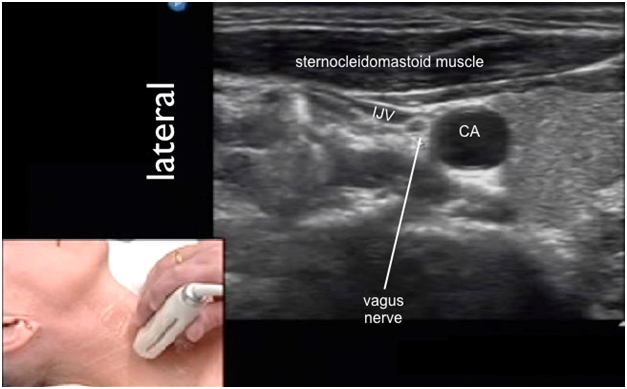
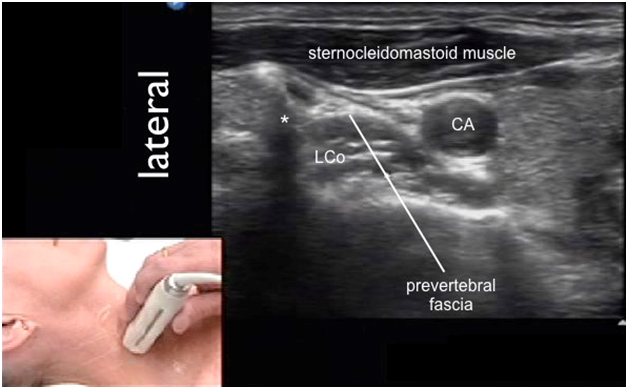
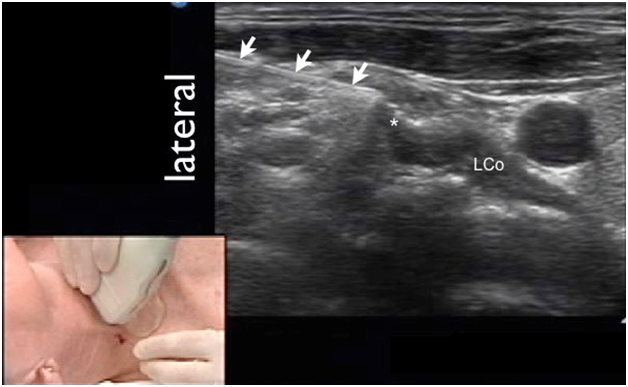
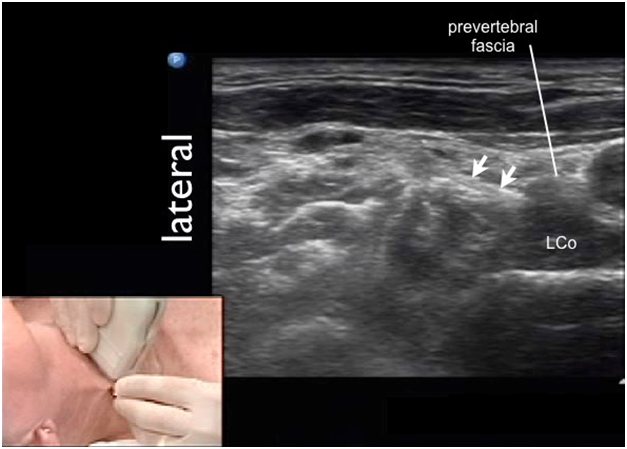
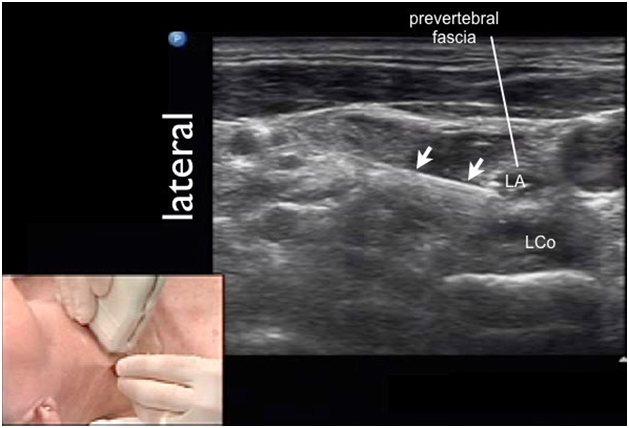
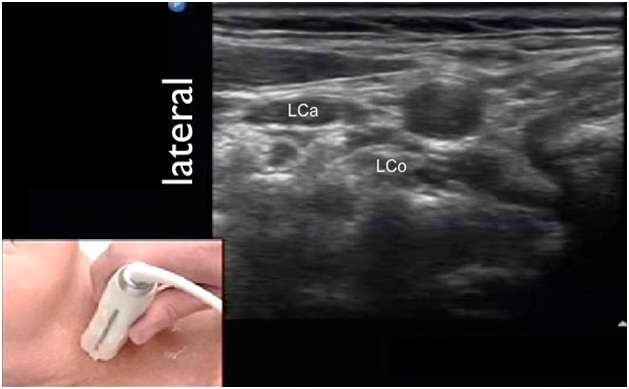
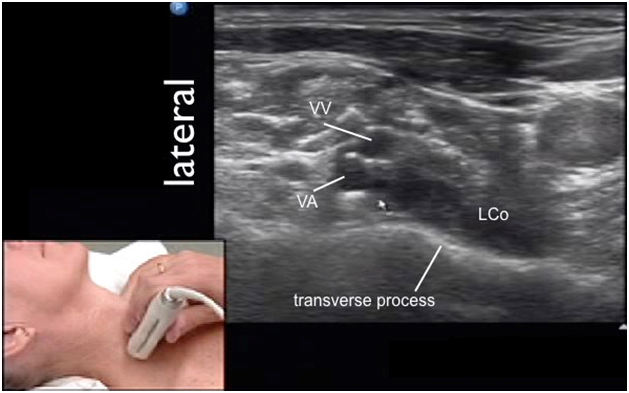
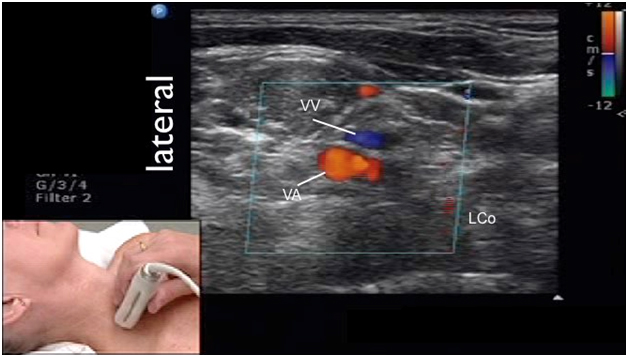
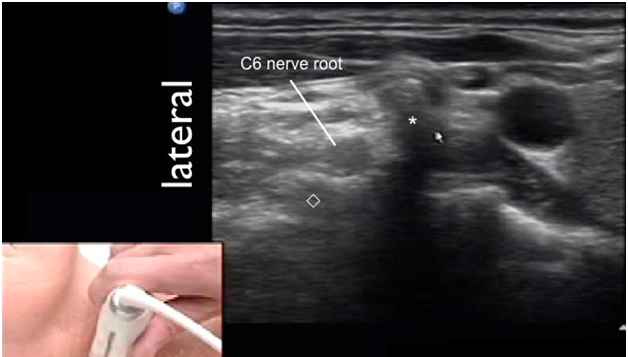
The prevertebral fascia is a layer of deep cervical fascia that envelops the prevertebral muscles (longus colli and longus capitis muscles) that attach to the cervical vertebral bodies and transverse processes (Figure 2). The cervical sympathetic trunk runs through the prevertebral fascia thus this important structure influences the extent of local anesthetic spread during stellate ganglion block. Success of the cervical sympathetic block relies on proper local anesthetic deposit deep to the prevertebral fascia.
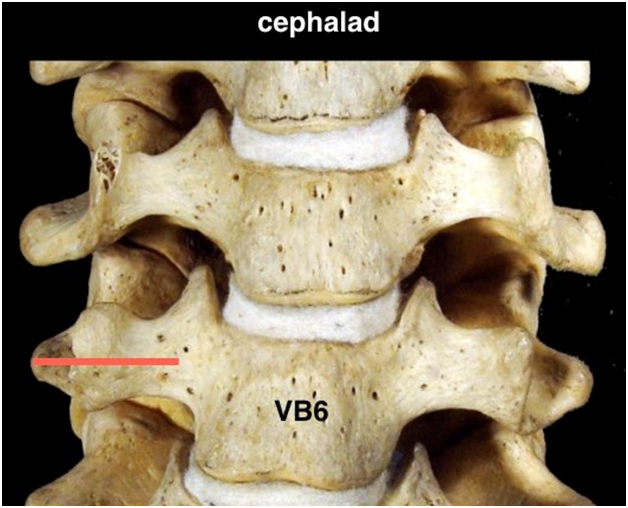
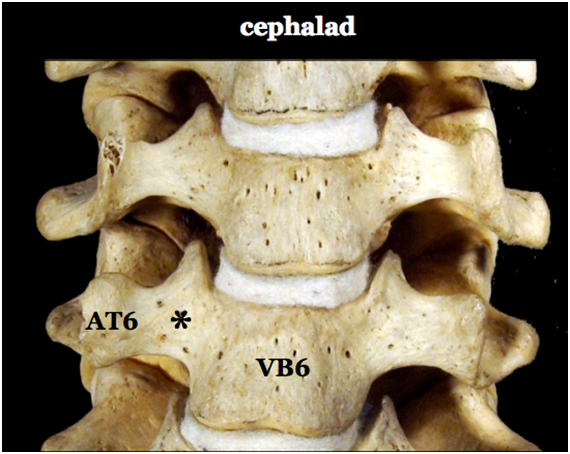
Figure 2. Anterior view of the cervical spine showing the C6 transverse process
|
AT6 = anterior tubercle of C6 transverse process VB6 = C6 vertebral body * = groove between TP and VB6 where longus colli muscle is located |
Movie 3. C6 transverse process anatomy