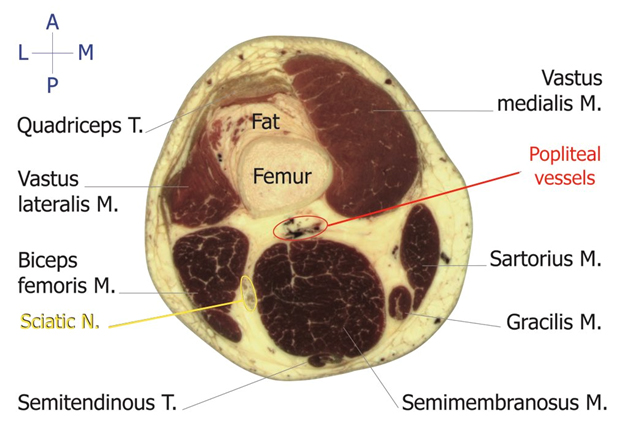
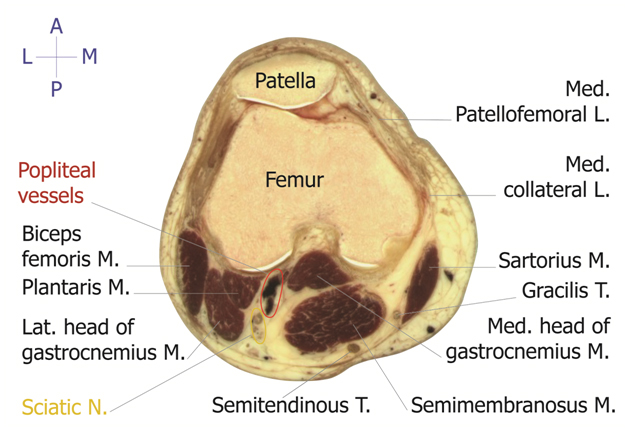
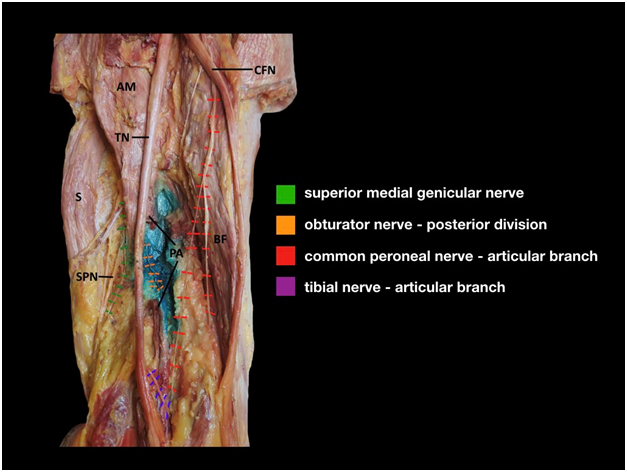
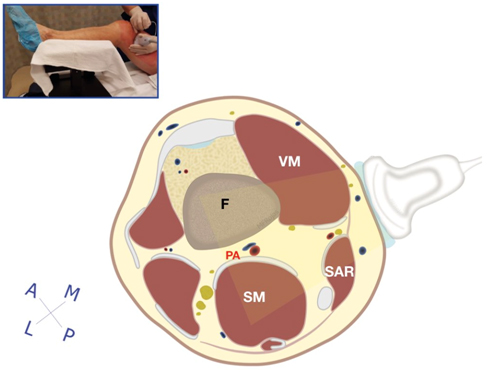
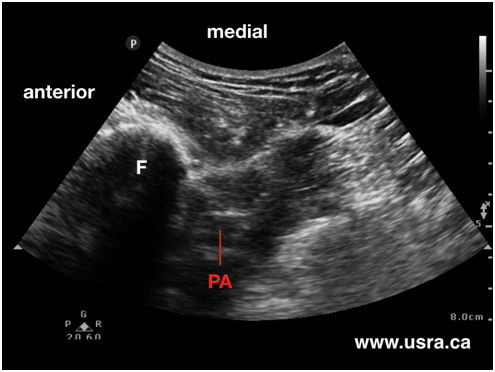
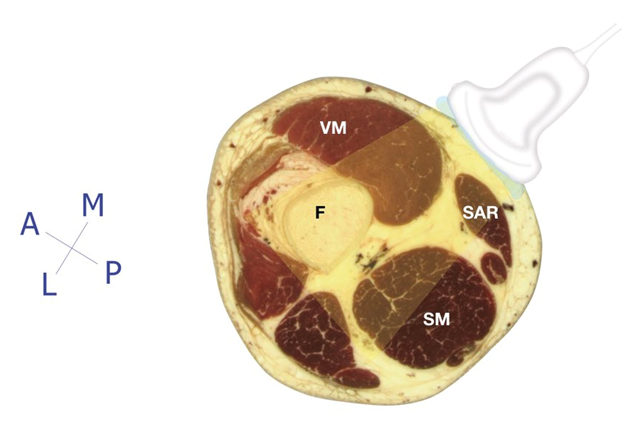
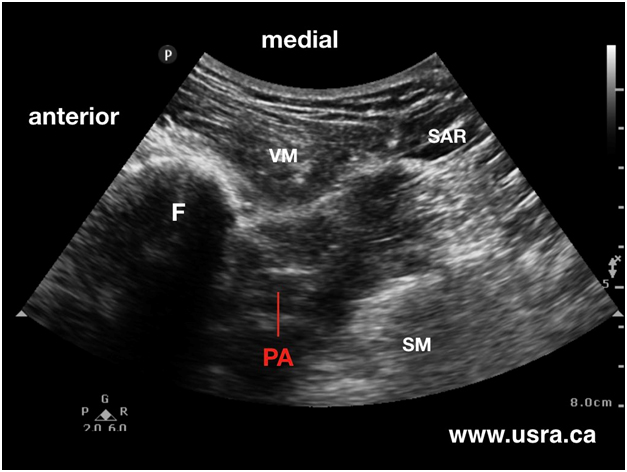
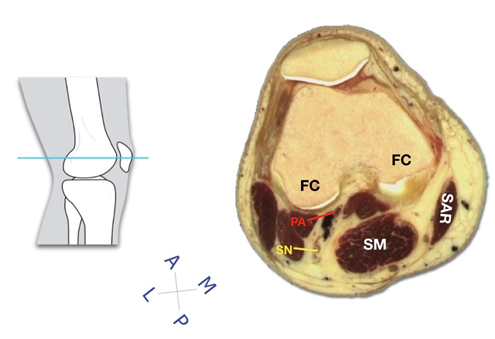
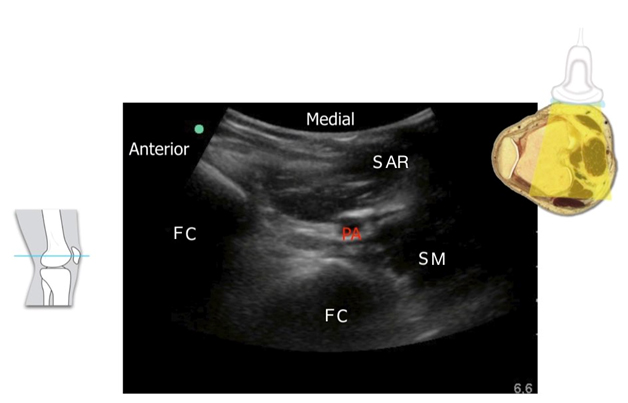
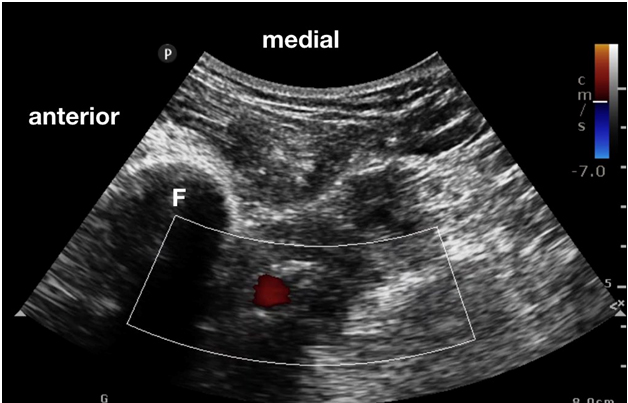
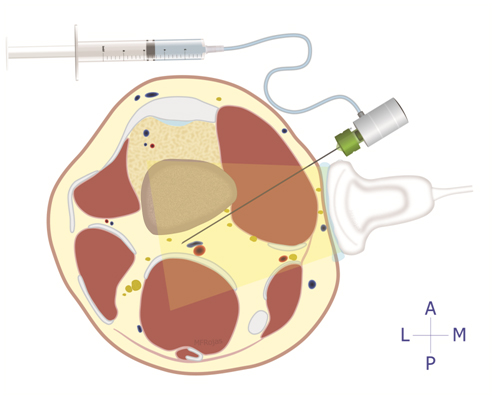
Background The concept of local infiltration analgesia (LIA) was first introduced by Kohan and Kerr to provide pain relief following total knee arthroplasty (TKA). Today, this simple, surgeon performed peri-articular injection under direct vision has become commonplace in clinical practice around the world. Up to 150 mL of local anesthetic solution (often ropivacaine 0.2%) containing a variety of adjuncts (epinephrine, NSAID, opioid, steroid) is injected during and at the end of TKA. The injection targets the anterior and posterior capsule of the knee, intercondylar area, collateral ligaments, tissue along the femur and tibia and the subcutaneous tissue. The analgesic effectiveness of the LIA technique is undisputed and has been confirmed in multiple clinical studies. The only drawback of single shot LIA is limited duration of analgesia (hours) unless liposomal bupivacaine is injected which can extend analgesia to up to 72 hours. Indwelling LIA catheter is not commonly applied because of the fear of infection. The iPACK block was first introduced by Dr. Sanjay Sinha. The acronym iPACK stands for infiltration between popliteal artery and capsule of the knee. The block is performed by anesthesiologists under ultrasound guidance to provide pain relief to the posterior aspect of the knee after TKA by blocking the articular branches of the tibial, common peroneal and obturator nerves in the popliteal region. The iPACK block likely achieves a similar degree of analgesia as posterior capsule injection as part of LIA performed by the surgeon. However, the iPACK block has a potential technical advantage over LIA injection since it is ultrasound guided and the needle path aims to stay clear of the popliteal artery and the sciatic nerve. In contrast, surgeons are often reluctant to inject deep into the posterior capsule for the fear of accidental popliteal artery puncture and sciatic nerve block since these posterior anatomical structures are not visualized anterior to the posterior capsule. At the time of writing, there is no randomized controlled trial to compare anesthesiologist performed iPACK with surgeon performed posterior capsule LIA with respect to analgesic effectiveness and duration.
Advancing the Science of Ultrasound Guided Regional Anesthesia and Pain Medicine