Scanning Technique
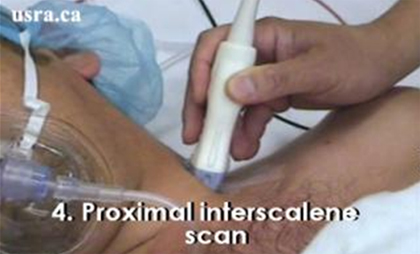
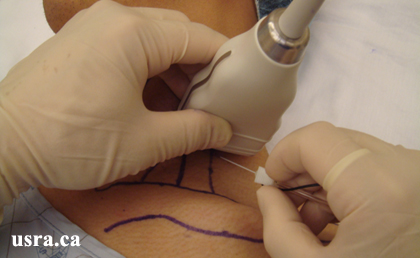
- Position the patient supine with the head turned 45 degrees to the contralateral side.
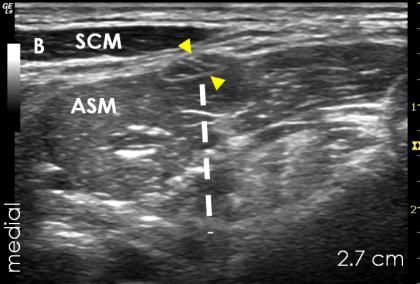
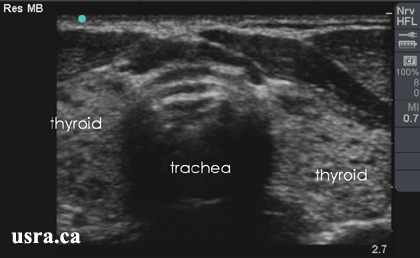
- After skin and transducer preparation (see Preparing Transducer for Single Shot), place a linear 38-mm, high frequency 10-15 MHz transducer firmly on the neck at the level of the cricoid cartilage in the axial, oblique plane to obtain the best possible transverse view of the brachial plexus.

|
Transducer over left interscalene region CL = clavicle |
- Optimize machine imaging capability by selecting the appropriate depth of field (within 2-3 cm), focus range and gain.
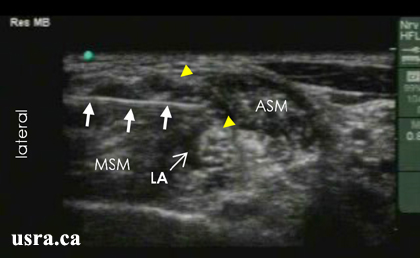
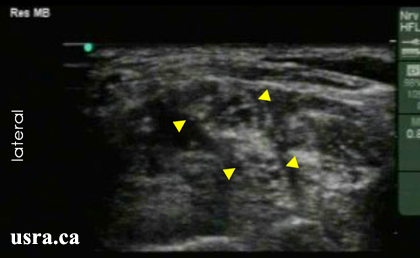
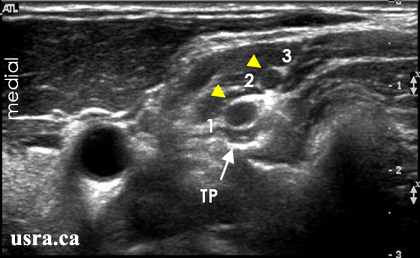
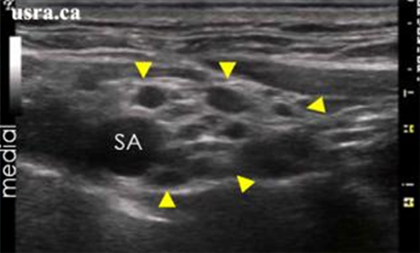
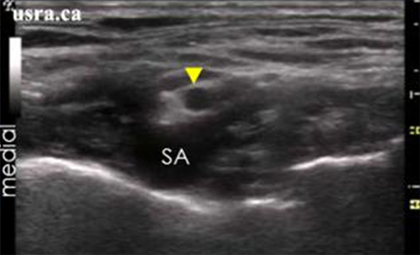
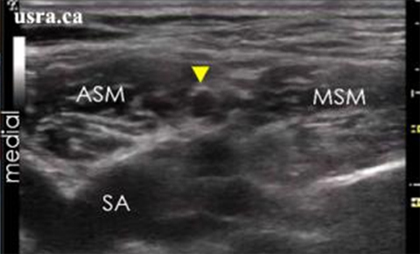
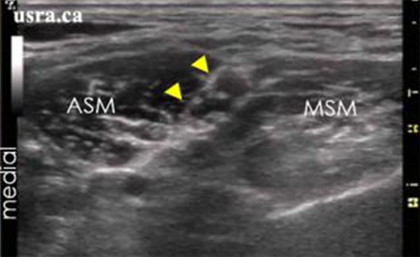
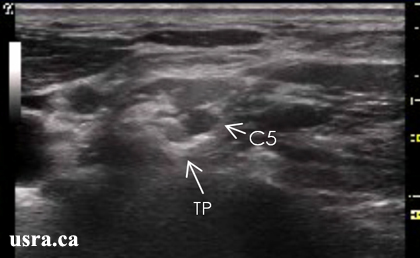
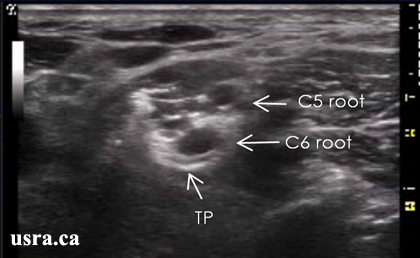
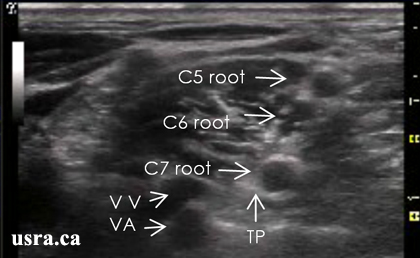
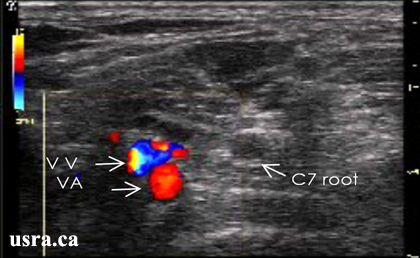
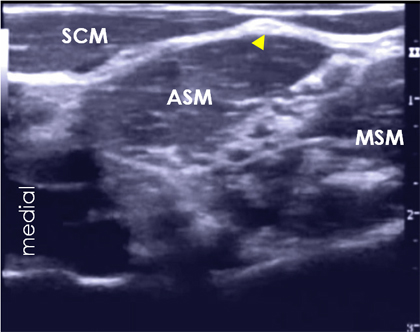
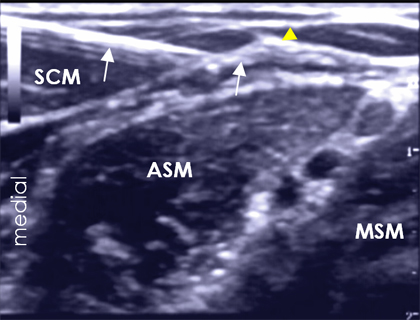
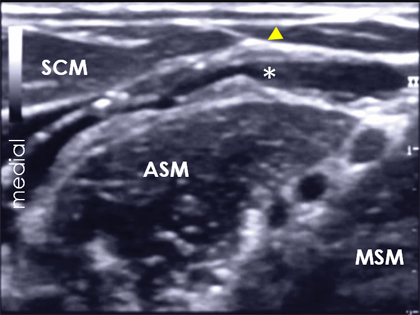
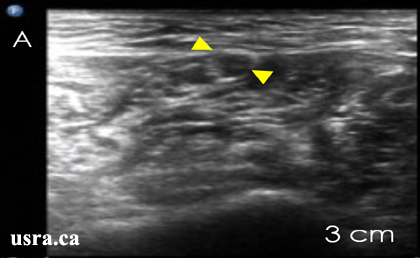
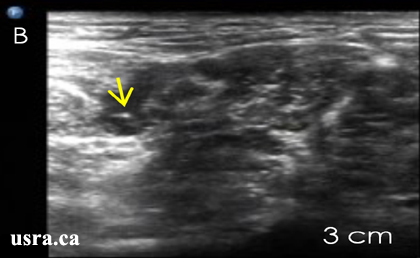
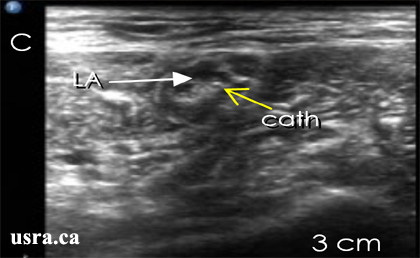
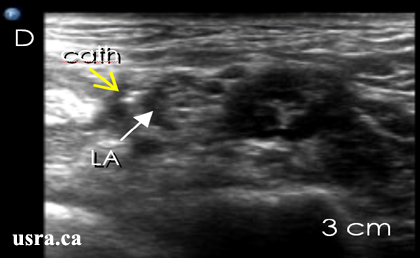
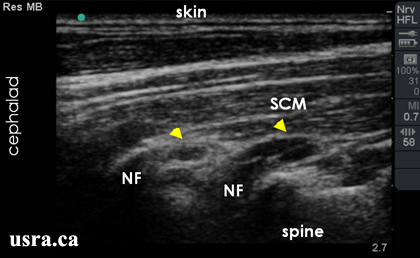
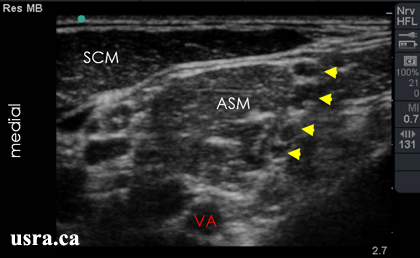
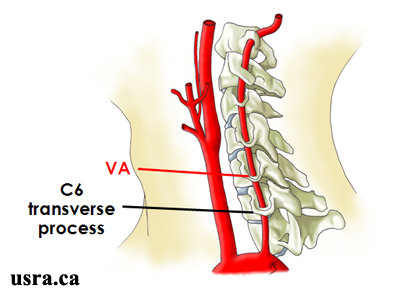
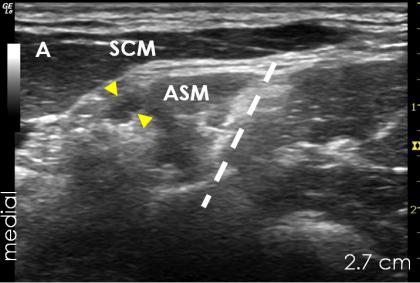
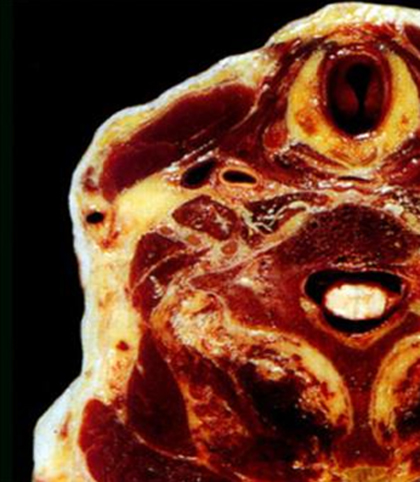
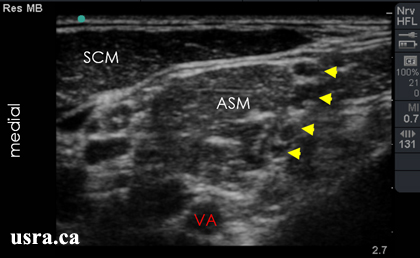
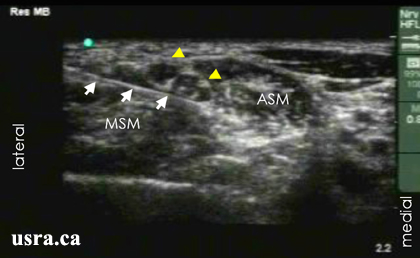
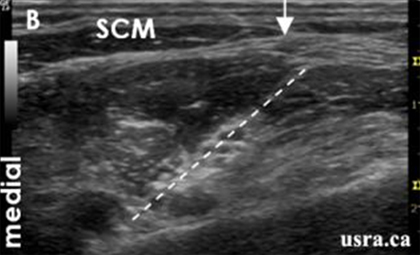
- Visualize the nerve roots or trunks in the transverse view (short axis). Nerves in the interscalene groove appear hypoechoic, distinctly round or oval, and are located between the anterior and middle scalene muscles. The internal jugular vein and carotid artery are visualized medially.

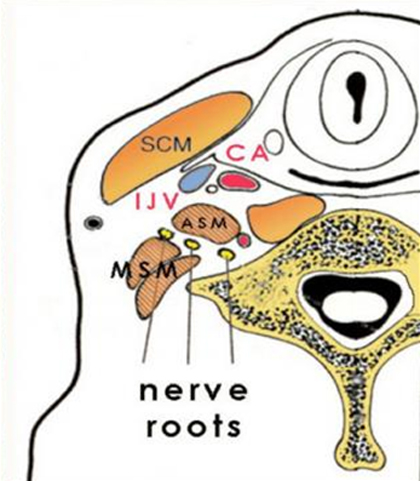
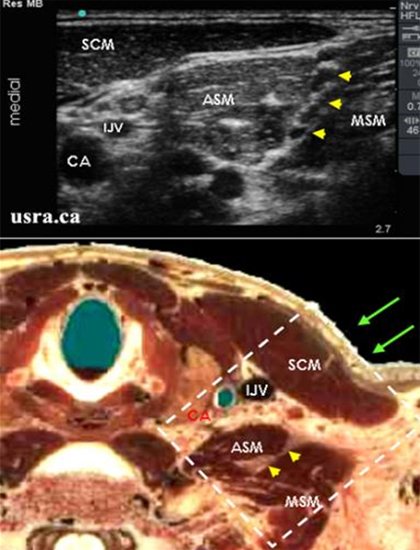
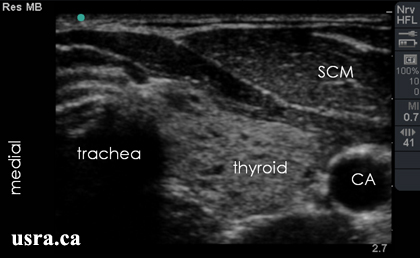

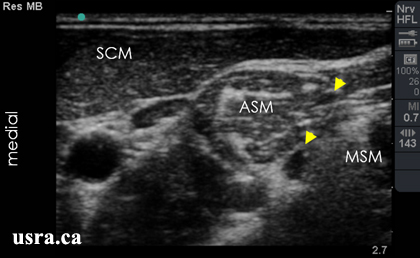
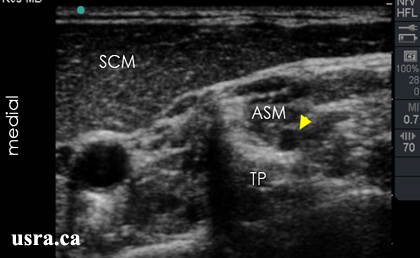
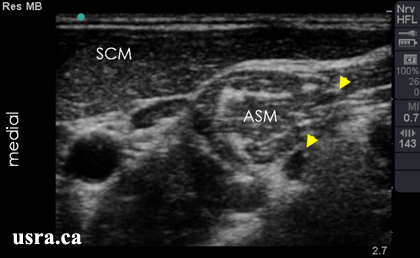

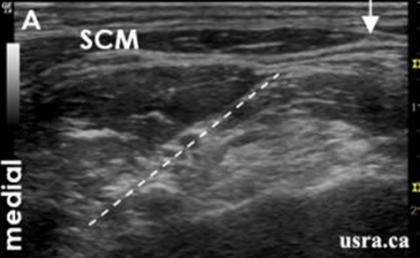
 SCM = sternocleidomastoid muscle
SCM = sternocleidomastoid muscle