Nerve Localization
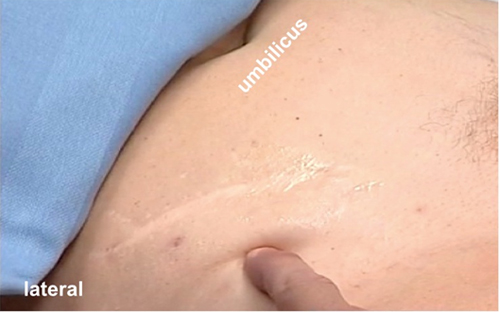
Palpable external landmarks that help to locate the LFCN are :
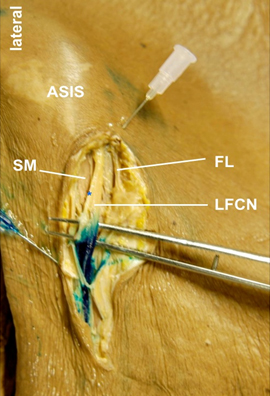
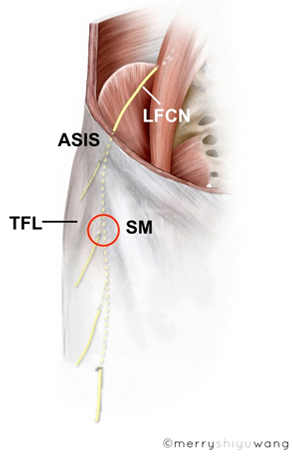
- the ASIS (Figure 4);
- the inguinal crease; and
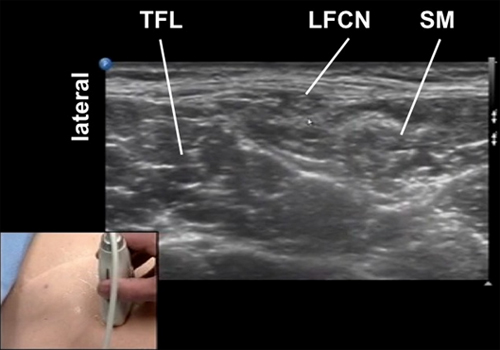
- a palpable groove between the SM and TFL muscle approximately 3 fingerbreadths caudad to ASIS (Figure 5).
Figure 4. Finger pointing at the anterior superior iliac spine, an obvious external landmark
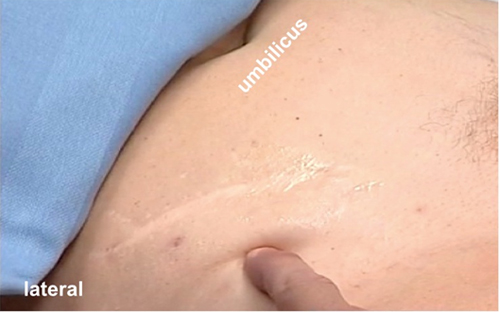
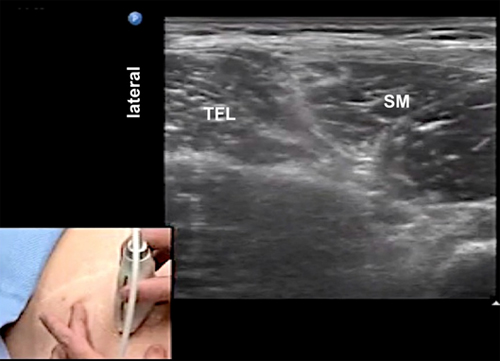
Figure 5. Initial transducer position over the groove between TFL and SM ~ 3 finger-breadths below the ASIS
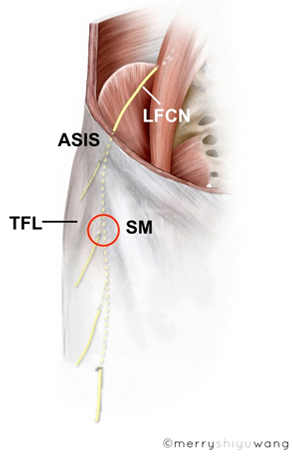 |
ASIS = anterior superior iliac spine
LFCN = lateral femoral cutaneous nerve
TFL = tensor fascia lata muscle
SM = sartorius muscle
O = ideal site to start scanning
|
The palpable groove between the SM and TFL muscle can be accentuated by asking the subject to actively flex the thigh.
A number of internal landmarks also help to locate and consequently trace the nerve proximally. They are:
- the SM medial and caudad to ASIS (Figure 6);
- the TFL muscle lateral and caudad to ASIS (Figure 6);
- a fat filed space between the SM and TFL muscle.
Figure 6. Sonogram showing internal landmarks caudad to the ASIS
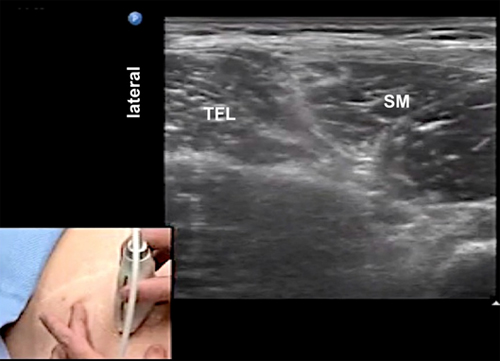 |
TFL = tensor fascia lata muscle
SM = sartorius muscle
|
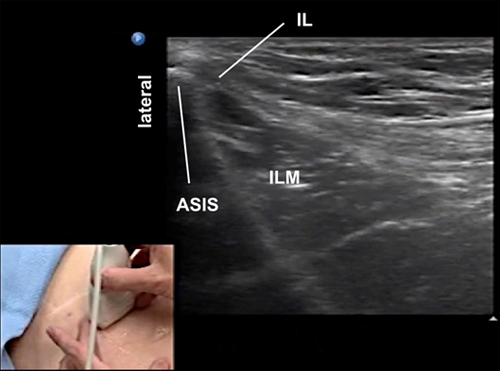
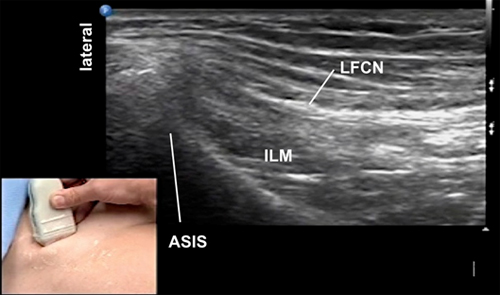
Also at the level of ASIS, thebony shadow of ASIS, the ilioinguinal ligament and the iliacus muscle are important internal landmarks for nerve localization (Figure 7).
Figure 7. Sonogram showing internal landmarks at the ASIS level
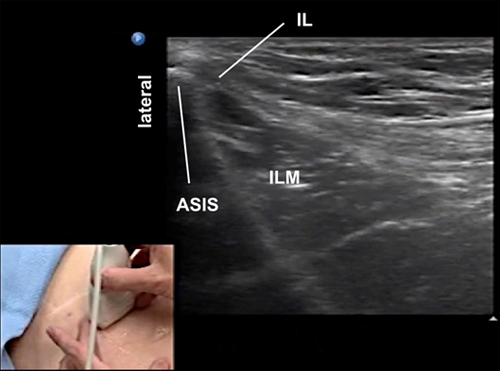 |
ASIS = anterior superior iliac spine
IL = inguinal ligament
ILM = iliacus muscle
|
The LFCN is a small nerve which can be challenging to locate and identify. This is particularly true near the ASIS. It is therefore advisable to trace the nerve starting distally and scan progressively cephalad.
After an initial palpation (ASIS and the groove between SM and TFL muscle), move the transducer (oriented transverse) to a site at least 3 fingerbreadths caudad to ASIS and search for the LFCN in the hypoechoic fat filled space deep to the fascia lata between the SM (medially) and TFL muscle (laterally).
This superficial fat filled groove is often flat, almond like or triangular in shape. It is interesting to note that similar compartments containing sensory nerves are commonly found throughout the body and they are called "fat filled flat tunnels."
The apparent size of this space is greatly influenced by the amount of transducer pressure applied to the skin. Again heavy transducer pressure will obliterate the space making visualization of the content difficult.
Within the space, the LFCN often has a honeycomb appearance and is regularly hyperechoic compared to the surround fat. It is often oval or spindle shaped.
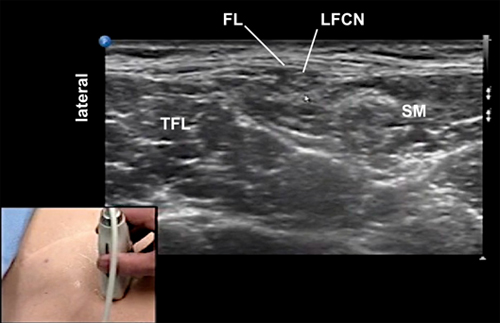
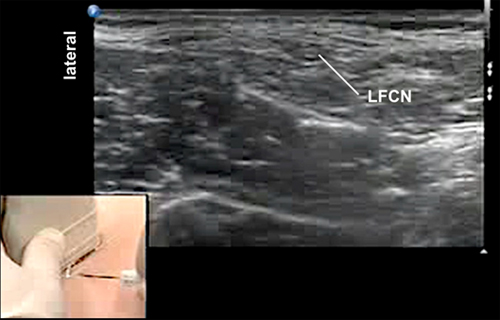
Aim to identify the fascia lata, the superior border of this space (Figure 8). Note that the nerve is subfascial and not subcutaneous.
Figure 8. Sonogram showing LFCN in the groove
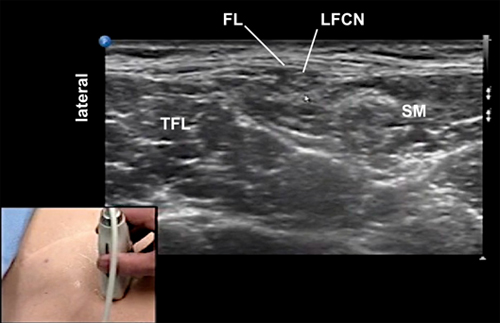 |
FL = fascia lata
LFCN = lateral femoral cutaneous nerve
TFL = tensor fascia lata muscle
SM = sartorius muscle
|
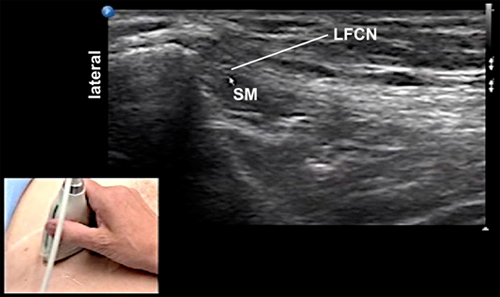
Once identified the nerve, move the transducer cephalad towards the ASIS to trace the LFCN to the anterior surface of the SM as the muscle becomes smaller and smaller at its attachment to the ASIS.
The echogenicity and shape of the LFCN may change depending on the level of scanning and the amount of fatty and/or connective tissue in a given individual.
More cephalad near to the ASIS, the nerve may become hypoechoic and more flat as it is now situated within connective tissue layers that have a minimum amount of hypoechoic adipose tissue (Figure 9). In case of two or more LFCNs or early branching of anterior division, each of these small nerves may appear as hypoechoic "bubble" (flat or round in shape) with white boundaries.
Figure 9. Sonogram showing a very flat LFCN at the level of ASIS
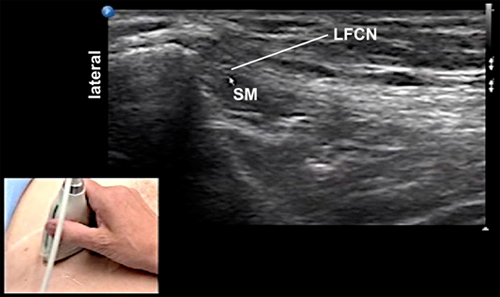 |
LFCN = a very flat lateral femoral cutaneous nerve lying on top of the sartorius muscle near ASIS
SM = the tendinous part of the sartorius muscleclose to itsattachment at the ASIS
|
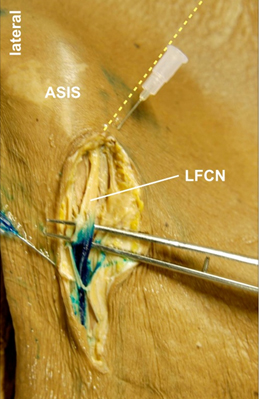
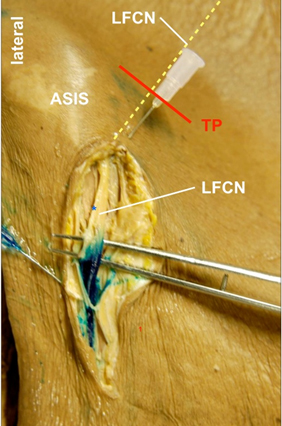
Note that it is technically challenging to image the LFCN immediately medial to or at the ASIS as the nerve crosses the inguinal ligament and makes almost a 900 turn from above the ASIS to below the ASIS (yellow broken line in Figure 10). Additionally, the nerve courses oblique in the pelvis before reaching the thigh (Figure 10). Due to numerous connective tissue layers and bone artifacts in this region, it is sometimes impossible to visualize the LFCN at this site.
Figure 10. The oblique course of the LFCN above the ASIS in the pelvis (yellow broken line)
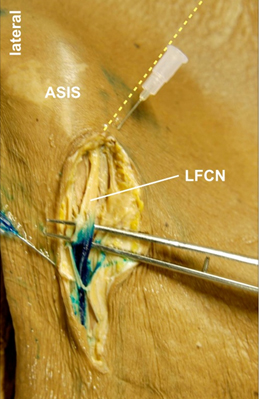 |
LFCN = lateral femoral cutaneous nerve
Yellow dotted line = oblique pelvic course of LFCN above ASIS
|
For this reason, it is necessary to change the transducer angle for imaging at or above ASIS. Casting the ultrasound beam to insonate the nerve at 90 degrees at this location can be difficult. This is the reason for a suboptimal image.