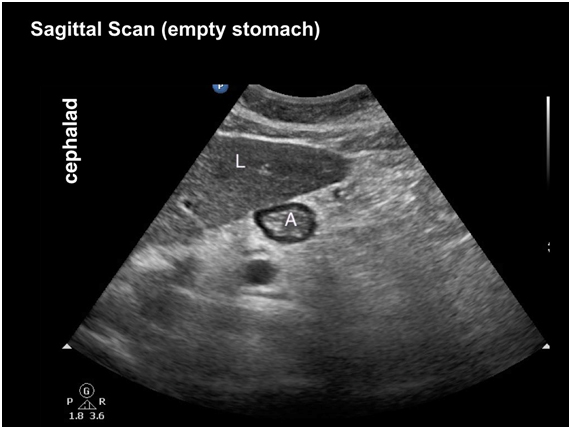
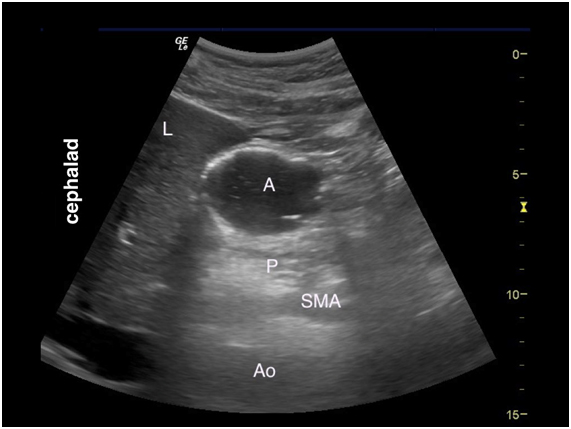
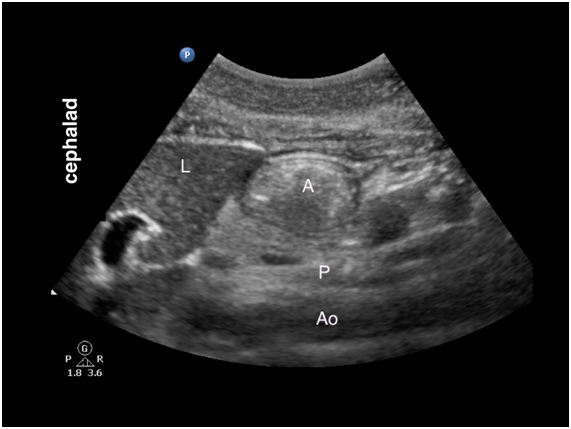
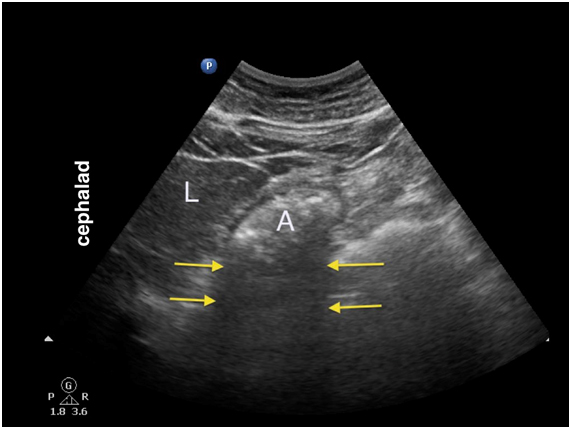
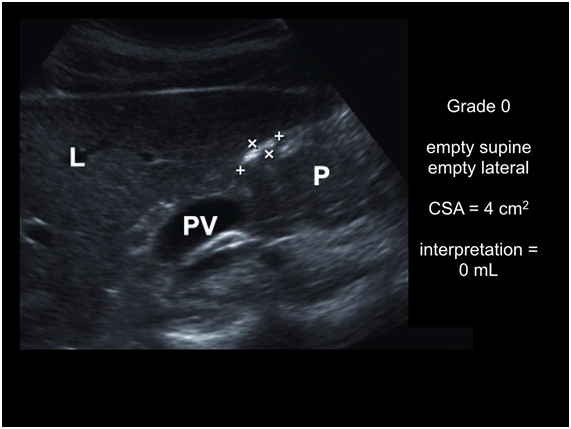
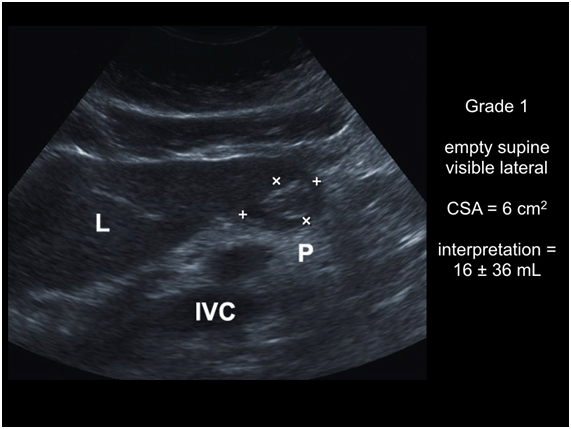
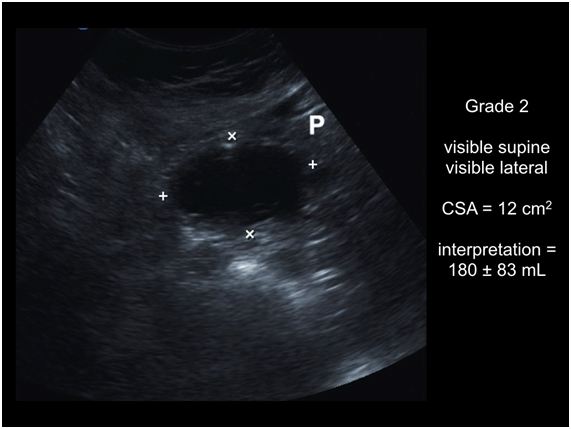
Introduction Pulmonary aspiration of gastric content is a major anesthetic-related complication which may result in significant morbidity and mortality. This is particularly true in high risk patients and situations e.g., parturients, emergency surgery, and diseases associated with slow gastric emptying. The volume, nature (fluid vs. particulate or solid matter), and acidity of the aspirate are thought to be important factors that determine patient outcomes. Current prevention strategies rely mainly on recommended fasting periods for elective surgery i.e., NPO protocol. However, underlying medical conditions that slow gastric emptying can predispose patients to greater amount of gastric content at the time of anesthetic induction despite appropriate fasting intervals. There is a growing interest in applying bedside ultrasound as a noninvasive portable tool to assess gastric content and volume to clinically evaluate aspiration risk by providing qualitative and quantitative information. The main objective of point-of-care (POC) gastric ultrasound is to help clinicians assess gastric contents when NPO status is unknown or uncertain in the immediate pre-anesthetic period. Other than anesthesiologists, POC gastric ultrasound is also useful to emergency physicians and intensivists who take part in sedation and airway management. It has a number of important features:
- it is a bedside, focused diagnostic examination
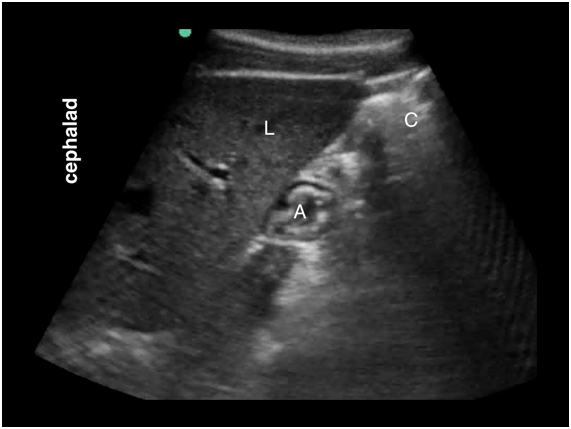
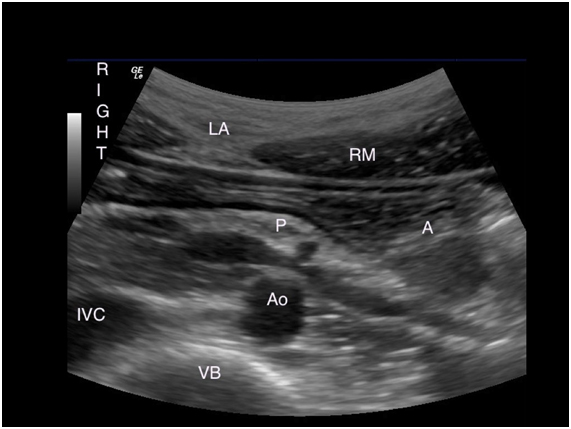
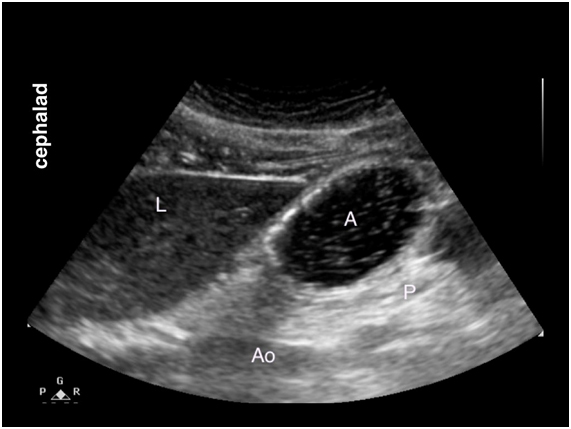
- it is a goal-directed assessment i.e., limited in scope and target structures
- the findings are easily recognizable
- the scanning technique can be quickly learned and performed
- the findings help to guide clinical care
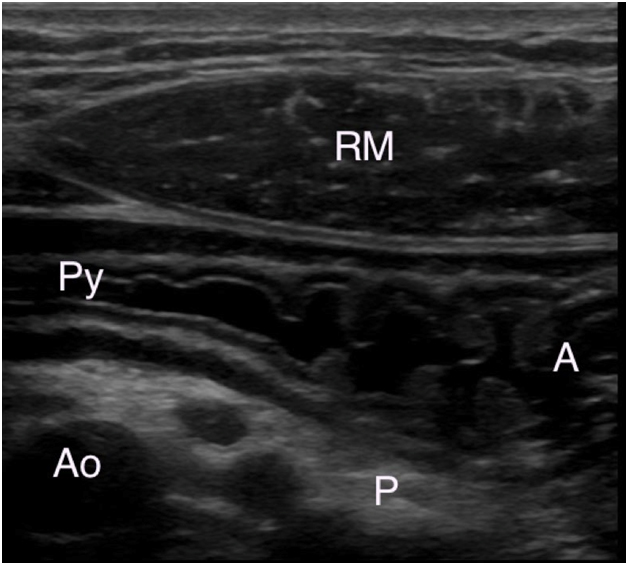
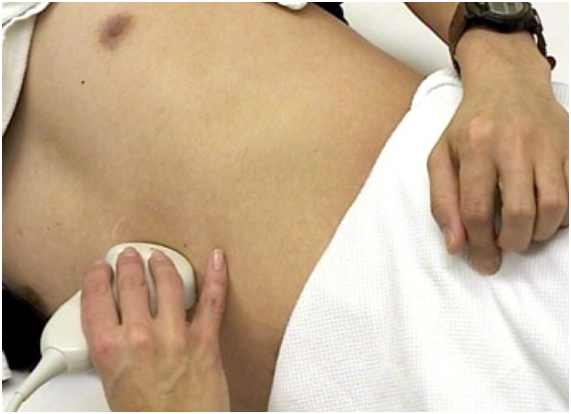
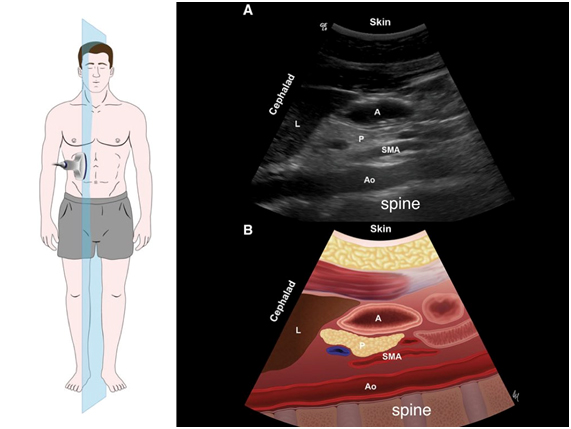
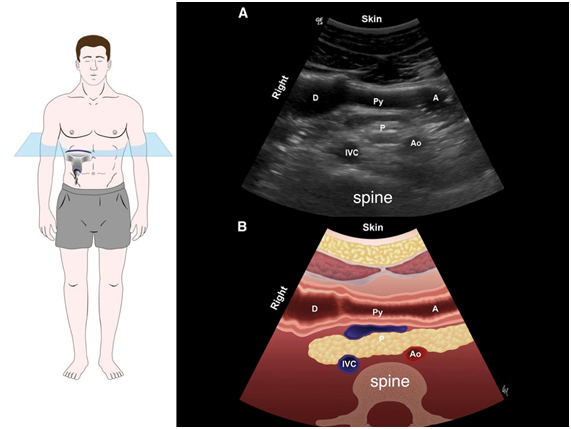
Point of care gastric ultrasound follows the I-AIM framework (I = indications, A = acquisition, I = interpretation and M = medical decision-making). This good framework describes the logical steps in performing and teaching gastric ultrasound. Acquisition of image requires selection of a proper probe (type, orientation), proper patient position, picture (image optimization) and examination protocol. Image interpretation involves interpretation of the anatomy, physiology, and artifacts. Finally, medical decision is made based on appropriate collaboration of ultrasound results with other physical examination, radiologic and laboratory test findings. It is important to acknowledge that a POC gastric ultrasound examination can conclusively rule in or rule out a clinical diagnosis. However, the ultrasound result may also be indeterminate in which case serial ultrasound evaluation is warranted. At the present time, research is ongoing to validate the diagnostic accuracy and clinical utility of gastric ultrasound in healthy and high risk patients undergoing elective and emergency surgery.