Anatomy
The GON is the sensory branch of the posterior ramus of the second cervical (C2) spinal nerve. Together with the lesser occipital nerve, the GON innervates the skin of the occipital region up to the top of the head (vertex).
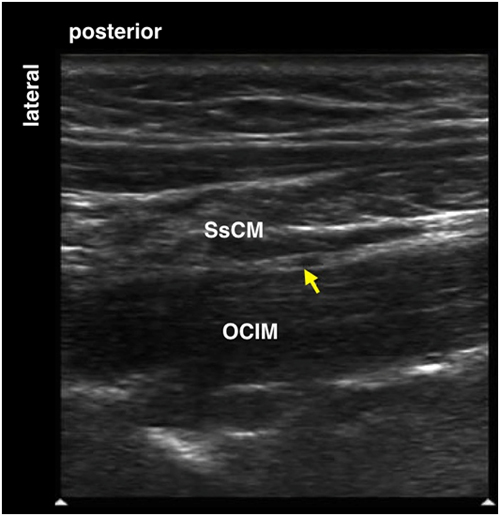
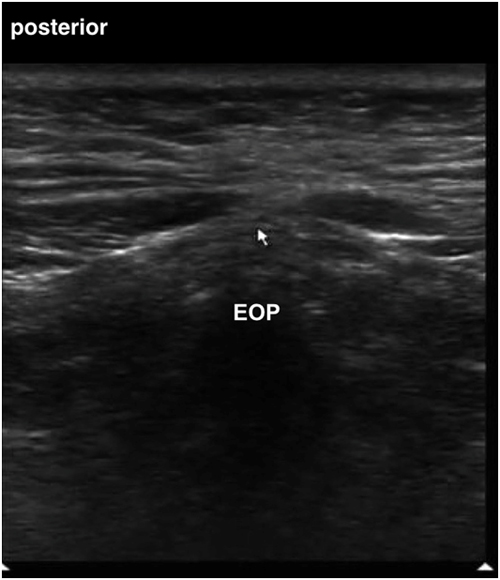
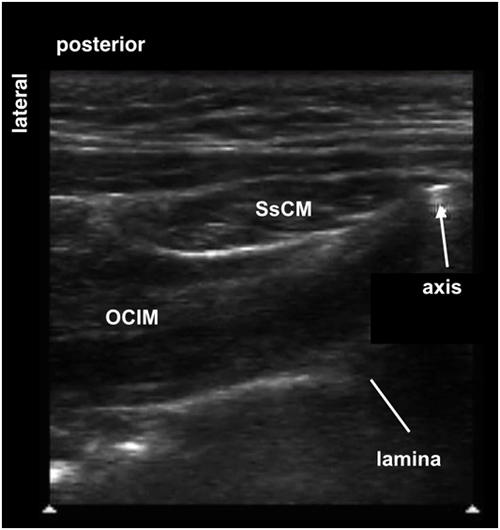
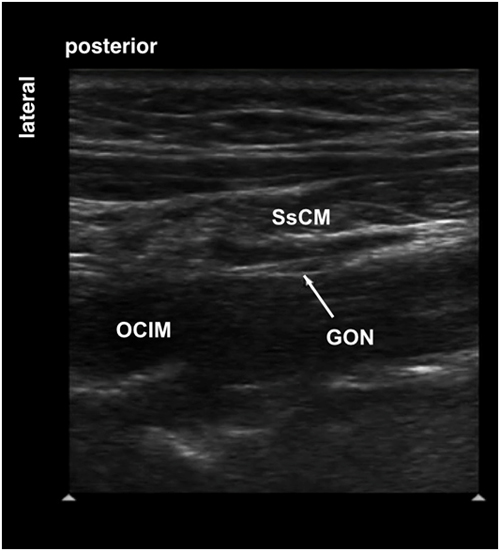
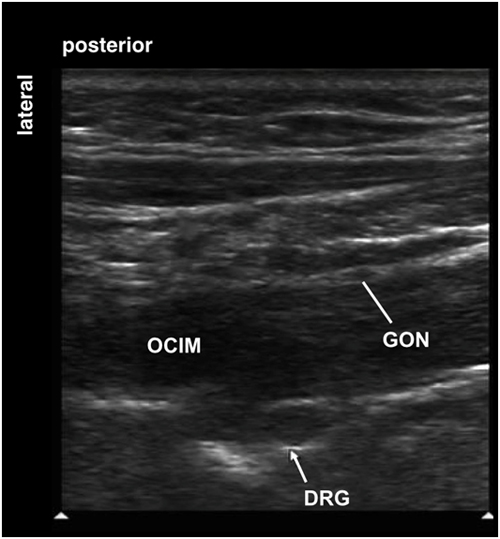
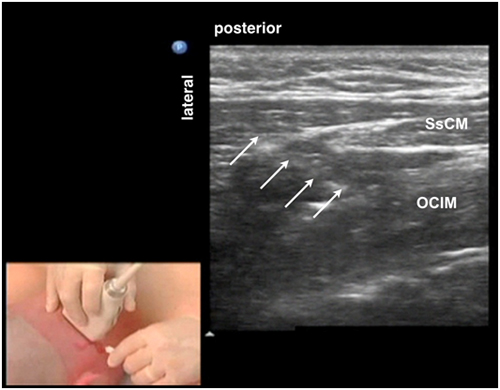
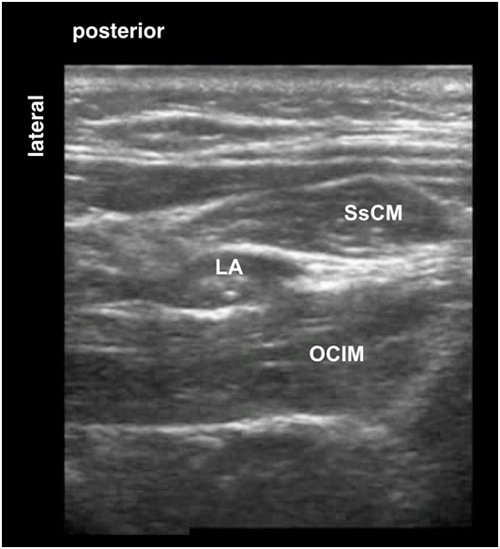
After leaving the C2 spinal nerve posterior to the lateral atlanto-axial joint, it travels inferiorly and laterally to appear at the inferior border of the obliquus capitis inferior muscle (OCIM). The GON travels in a fascial plane between the OCIM and the semispinalis capitis muscle (SsCM) as it ascends on the posterior surface of the OCIM before it pierces (SsCM). The GON terminates as a superficial nerve by either piercing the upper part of the trapezius muscle or running through the tendinous arch between the trapezius muscle and the sternocleidomastoid muscle, where it lies medial to the occipital artery.
The suboccipital triangle is formed by three muscles, the obliquus capitis inferior muscle, the obliquus capitis superior muscle and the rectus capitis posterior major muscle (Figure 1).
Figure 1. Anatomy of the right suboccipital triangle in the posterolateral aspect of the neck
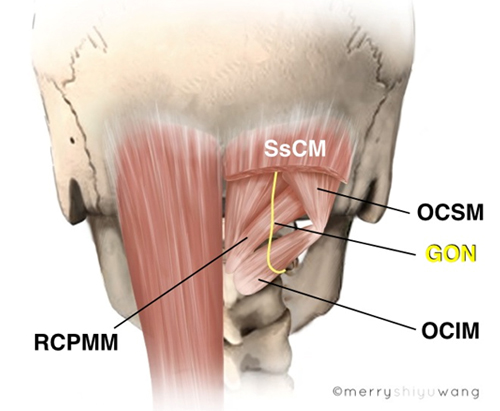
|
GON = greater occipital nerve OCIM = obliquus capitis inferior muscle OCSM = obliquus capitis superior muscle RCPMM = rectus capitis posterior major muscle SsCM = semispinalis capitis muscle |
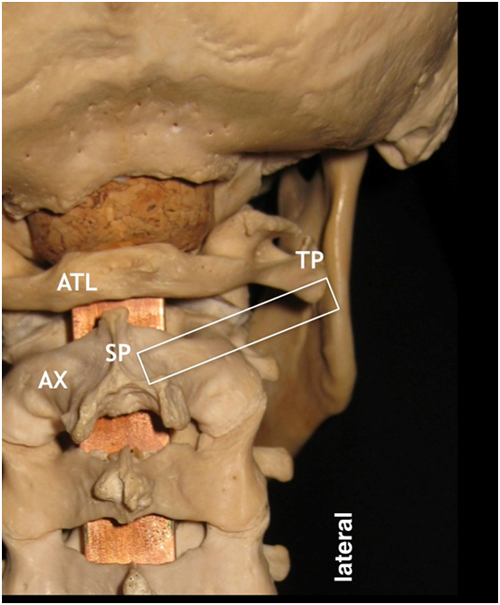
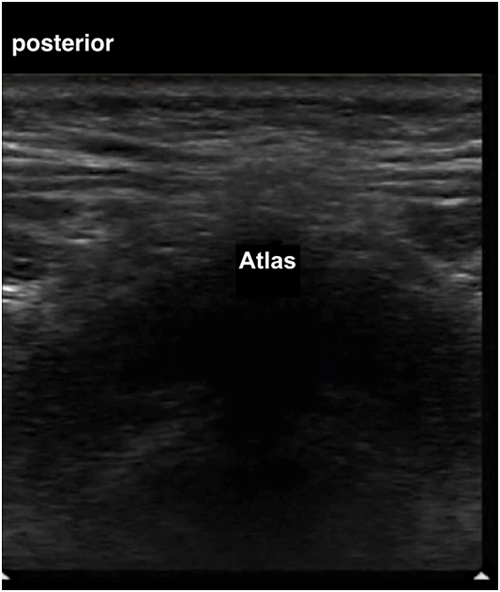
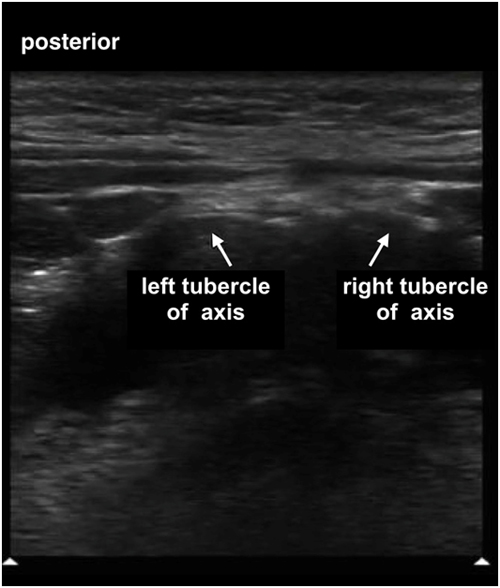
The OCIM is the important deep muscular landmark for localizing the GON. The right OCIM spans from the spinous process (right tubercle) of the axis (C2) medially to the transverse process of the atlas (C1) laterally (Figure 2).The RCPMM spans from the spinous process (SP) of the axis to the lateral part of the inferior nuchal line of the occiput.
The OCSM spans from the transverse process of the atlas to the occiput, slightly superior and lateral to the inferior nuchal line (Figure 2).
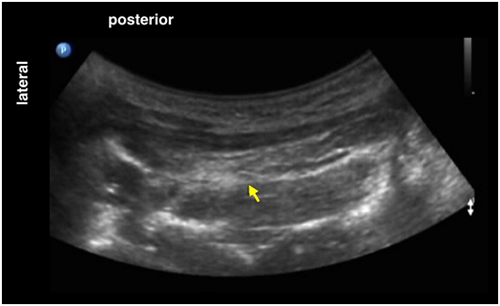
Figure 2. Cadaver specimen showing the right suboccipital triangle in the posterolateral aspect of the neck with the semispinalis capitis muscle removed
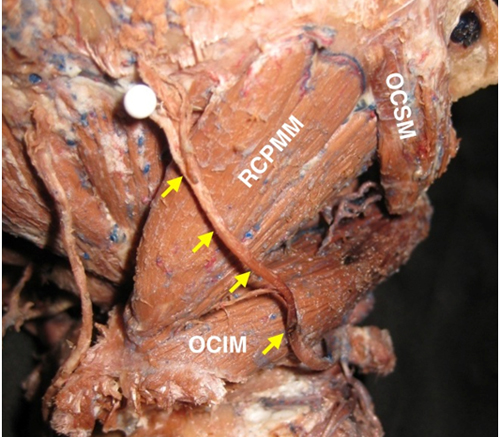
|
yellow arrows = greater occipital nerve OCIM = obliquus capitis inferior muscle OCSM = obliquus capitis superior muscle RCPMM = rectus capitis posterior major muscle |
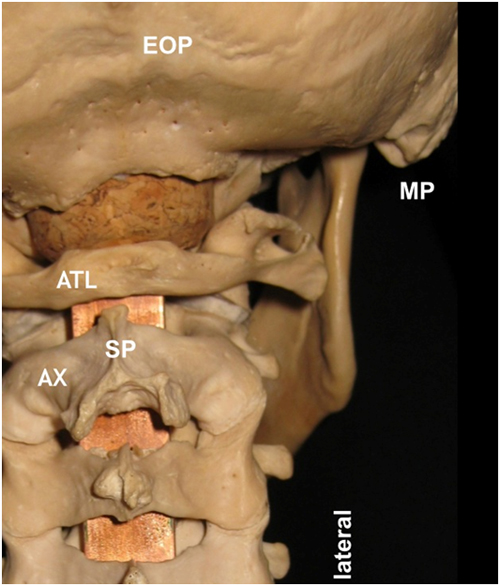
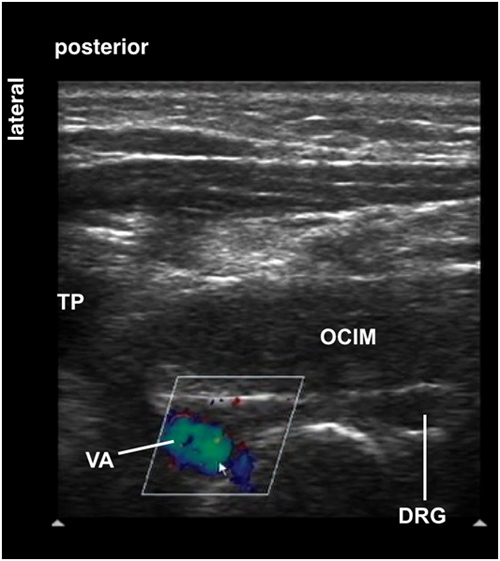
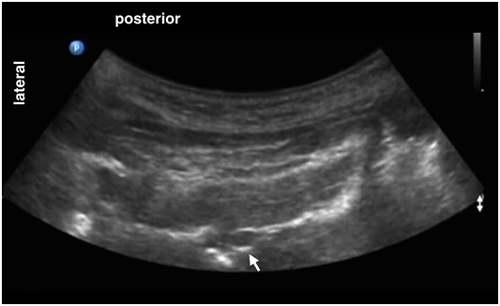
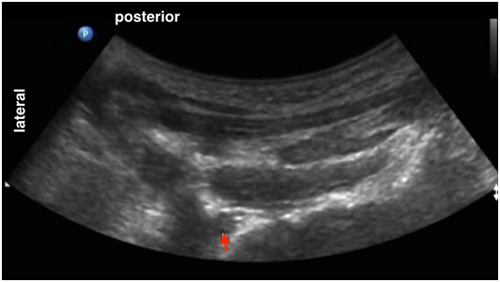
It is important to recognize the vertebral artery (VA) when performing GON block. Before entering the suboccipital triangle, the VA is located anterior to the OCIM at this level and is in close proximity to the transverse process (TP) of the atlas. Note that the VA is significantly lateral to the GON (Figure 3).
Figure 3. Location of the vertebral artery relative to GON
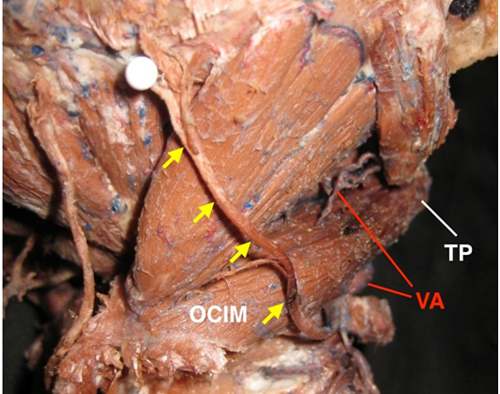
|
yellow arrows = greater occipital nerve OCIM = obliquus capitis inferior muscle TP = transverse process of the atlas VA = vertebral artery |
After ascending through the foramen transversarium of C1, the vertebral artery reaches the suboccipital triangle (upper red open arrow) and passes through a groove over the posterior arch of the atlas before entering the foramen magnum.