Anatomy
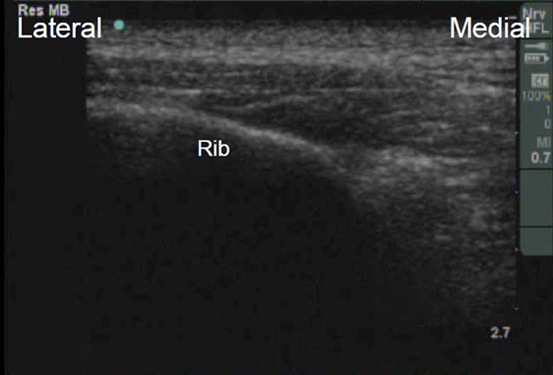
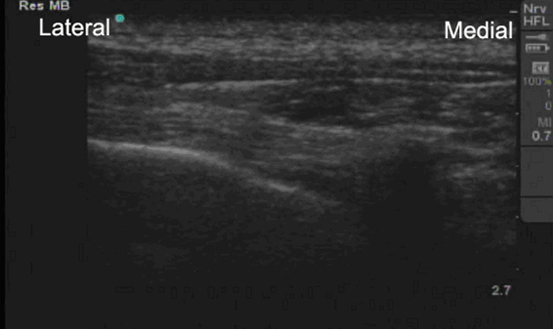
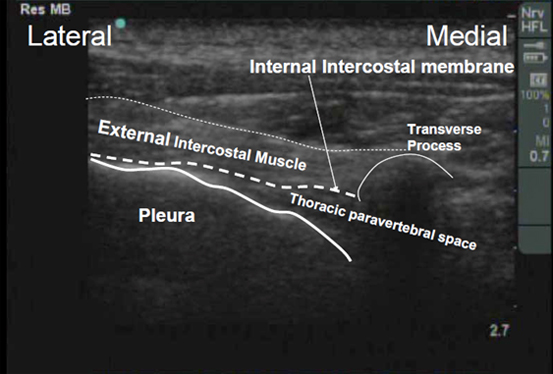
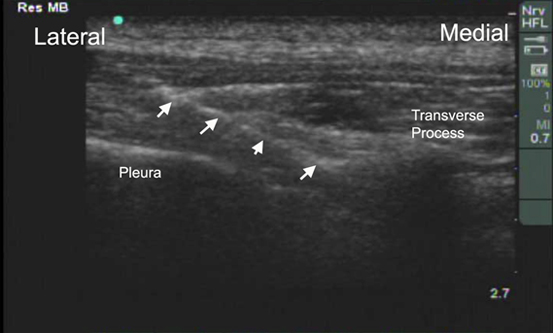
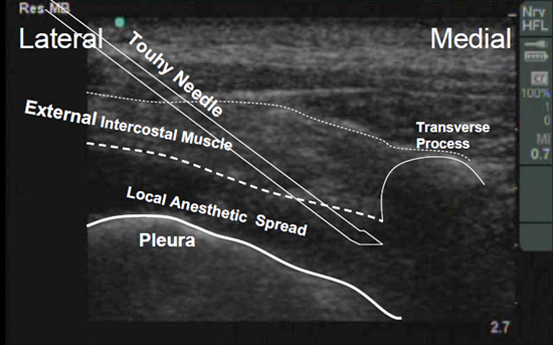
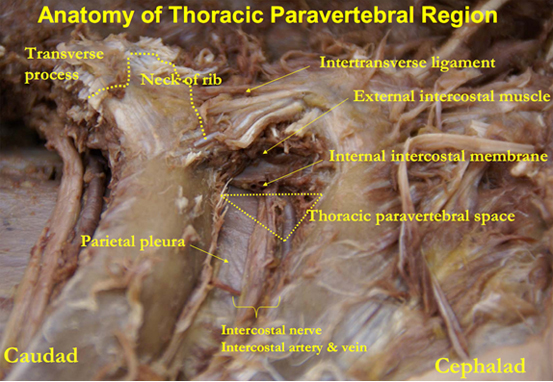
The thoracic paravertebral space (TPVS), when viewed in transverse cross-section
is triangular-shaped (red triangle in figure below). The base is formed by the
posterolateral aspect of the vertebral body / intervertebral discs / intervertebral
foramina / articular processes. The anterolateral border is formed by the parietal
pleura, whilst the posterior border is formed by the superior costotransverse
ligament. This ligament extends from the inferior aspect of the transverse
process above to the superior aspect of the rib tubercle below. Lateral to
this ligament (and continuous with it) is the internal intercostal membrane,
which is the aponeurotic continuation of the internal intercostal muscle,
and thus runs between the upper and lower border of adjacent ribs.12
The apex of the triangular TPVS communicates with the intercostal space laterally.
The cephalad limit of the TPVS has not been defined. It has been shown
that solution injection into the TPVS can spread caudad into the
abdominal and lumbar region, through the medial and lateral arcuate
ligaments of the diaphragm. It is generally accepted, however, that
the caudad limit of the paravertebral space is at the origin of the psoas
muscle at L1.9
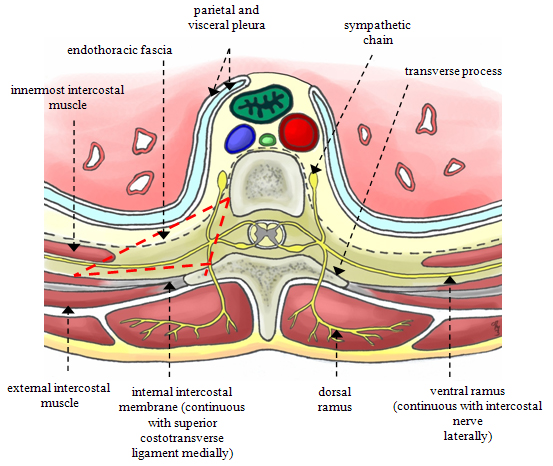
The TPVS contains mainly fatty tissue, and is traversed by the intercostal or
spinal nerves, intercostal vessels, dorsal rami, rami communicantes, and the
sympathetic chain. The spinal nerves do not have a fascial sheath in the TPVS,
which explains their susceptibility to local anesthetic blockade.
The space is divided into an anterior and posterior compartment by a fibroelastic
membrane, the endothoracic fascia. The endothoracic fascia is the deep investing
fascia of the thoracic cavity. It blends medially with the periosteum of the
vertebral body; and laterally, is closely applied to the ribs. Caudally,
it is continuous with the transversalis fascia of the abdominal cavity and
this may explain why solutions injected in the TPVS may spread to the
lumbar region. The spinal nerves have been described as running through
the compartment posterior to the endothoracic fascia.2 This
however is controversial,10,11 as the precise anatomy of the
endothoracic fascia, and its relationship to the spinal nerves in
particular, remains ill-defined. It has been shown that injection closer
to the spinal nerves (using a nerve-stimulator-guided technique) is more
likely to result in longitudinal spread of the injectate in the TPVS.11
Advancing the Science of Ultrasound Guided Regional Anesthesia and Pain Medicine